Last month, this blog discussed the managed care organization (MCO) scorecards created with review data collected by MetaStar. These scorecards enable enrollees in Wisconsin’s Home and Community-Based Services (HCBS) programs to easily compare MCOs and select one that has been fairly and impartially reviewed. There is another program that falls under Medicaid HCBS in Wisconsin: Include, Respect, I Self-Direct (IRIS). Since 2008, the IRIS program has operated as a self-directed program by the enrollee. “That means you will have the freedom to decide how you want to live your life,” says the WI DHS website. That freedom and independence is important to those who enroll in the program.

Preserving independence can be crucial for older individuals and people with disabilities. According to an article in the International Journal for Equity in Health, “Preservation of independence is among the most important health priorities cited by older adults” (Enogela, Buchanan, et al 2022). Additionally, less independence can lead to increased depressive symptoms in patients with spinal cord injuries and vice versa (Monin, Schulz, et al 2015). We all want to keep our independence and ability to care for ourselves as long as possible. The IRIS program provides more control for enrollees over their care and decisions affecting their bodies, homes, and lives.
Studies have also shown that aging-in-place, or allowing individuals to age at home, provides many benefits, including routine, comfort, and reduced physical and mental strain. The same holds true for those with disabilities. However, most healthcare insurance companies don’t cover the services and needs of older individuals or persons with a disability living in their home. The HCBS waiver allows IRIS enrollees to remain in their home and receive the necessary healthcare and other services, reducing hospitalizations and assisted living fees and preserving their independence.
The IRIS Difference
HCBS programs, such as Family Care (FC), Family Care Partnership (FCP) and the Program of All-Inclusive Care for the Elderly (PACE), use MCOs to coordinate care for enrollees. However, the IRIS program empowers enrollees by allowing them to manage their own care. They are given a budget based on their current needs and long-term goals, and they can spend that money however they see fit within the program’s rules and regulations. IRIS covers a variety of services and commodities, including in-home medical care, house cleaning, errands, assistive devices, and more.
WI DHS’s IRIS website points out, “Joining IRIS does not mean doing things all by yourself. Others will help you along your way.” Others include an IRIS consultant and a fiscal agent, who can advise the enrollee on how to use the budget for current needs and adjust it when future needs arise.
Wisconsin’s IRIS program has over 25,000 people enrolled as of January 1, 2024 (WI DHS). Each individual selects an IRIS consultant agency (ICA) to work with—an important decision essential to smooth and safe service. How can enrollees effectively compare these organizations to determine which one is right for them? Enter MetaStar. MetaStar is essential in upholding IRIS program standards and providing user-friendly scorecards for each ICA, helping enrollees easily determine which ICA to work with.
MetaStar’s ICA Review Process
ICAs have different responsibilities to their participants than MCOs, resulting in different review processes. The IRIS program review focuses on the interactions between the enrollee, consultant, and ICA.
The MetaStar IRIS Record Review team, part of the External Quality Review Department, evaluates the six IRIS consultant agencies in Wisconsin. As noted in the previous blog post, this team is populated by former care workers, including social workers, nurses, and therapists who “come with direct experience in the field and really understand how the system works,” said Alicia Stensberg, MetaStar Project Manager.
The MetaStar IRIS Record Review team reviews over 400 ICA participant files quarterly, looking for a comprehensive care plan, monthly contact by the IRIS consultant with the participant, incident documentation, and other quality indicators. Data collected is converted into scorecards by WI DHS. “It’s a lot of oversight at the participant level to make sure their needs are getting met.” explains Stensberg. The MetaStar IRIS Record Review team helps to make sure the ICAs understand the metrics and requirements. They also provide technical assistance and help solve problems during the review process.
MetaStar’s team helps organizations address “not met” requirements by clarifying requirements, monitoring follow-ups, and documenting improvements. “We have a lot of contact with these organizations,” Stensberg said. “We also work closely with the state to make sure the ICAs are improving, and they are.” She notes that while immediate improvements may not be evident each quarter, significant long-term enhancements in the performance of the ICAs have been seen, which she attributes, in part, to the ongoing reviews.
Hotline for IRIS Participants
MetaStar also operates a hotline for IRIS participants to report grievances or complaints regarding the IRIS program. MetaStar employees staff the hotline during business hours. The MetaStar employee works with the participants and the agencies to find acceptable resolutions. “From a statewide perspective, the [number of] grievances is relatively low, less than 1% of the membership,” Stensberg said. “It’s a healthy amount. No grievances mean people aren’t exercising their rights.” The grievances reported during these calls do not affect the scorecard results.
The IRIS program supports Medicaid enrollees’ dignity and independence. MetaStar provides clear evaluations of the ICAs and a grievance hotline, ensuring enrollees’ care is taken seriously. It’s crucial to consider future medical and personal care—for oneself and loved ones. “Anyone can end up needing Medicaid benefits at any time,” Stensberg explains. She also reminds us that “one of the most important things that we can do as a society is take care of the people who are marginalized. It is our duty, and frankly, it would cost us a heck of a lot more if we didn’t.” Scorecards created by WI DHS with data from MetaStar’s experienced review team enable clear decision-making during difficult times and offer a way for WI DHS and MetaStar to help Wisconsin’s marginalized populations.
“Do not regret growing older,” said Mark Twain. “It is a privilege denied to many.” While we’re not entirely sure Mark Twain is the author of this adage, the truth in the statement still rings clear: aging is not a disease to be fought, but a stage of life to appreciate and possibly even enjoy. However, aging can also bring health issues, loss of ability, financial struggles, and lack of a support system. By 2040, the number of Americans age 65 and older will reach 21.6%, according to the Administration for Community Living (ACL), up from 16% in 2000. Additionally, people who are disabled—who make up almost 27% of the population according to the United States Centers for Disease Control and Prevention—experience similar challenges.
These groups of people often face challenges caring for themselves. While some lucky people can self-fund care in aging years or disability, many others lack the financial resources for these situations. While Medicare and private insurance can alleviate medical costs and replace lost wages, medical care isn’t the only need to arise when a person becomes unable to care for themself.
Medicaid enrollees receive medical care, but they also require support in their homes and communities for various tasks, including at-home medical tasks, personal care, home care, pet care, errands, and much more. However, most health insurances won’t cover these services outside of a medical setting. Older adults or people with a disability are then caught in a web of problems: Can they self-pay for care? Is there a friend or relative who can help them? Should they move to a nursing home or assisted living facility? Depending on the extent of needs, some of these options aren’t possible. Fortunately, Wisconsin offers various ways to meet the long-term care needs of older adults and people with disabilities while allowing them to stay in their own homes.
The Wisconsin Way of Meeting Long-Term Care (LTC) Needs
Wisconsin provides LTC services through Medicaid Managed Care programs, including Home- and Community-Based Services (HCBS), through the following programs: Family Care (FC), Family Care Partnership (FCP), and the Program of All-Inclusive Care for the Elderly (PACE). FC is offered statewide while FCP and PACE are only offered in certain counties. These programs, operated by managed care organizations (MCOs), provide a variety of healthcare and other services that allow people to remain in their homes. When a person enrolls in one of the HCBS programs, they need to choose an MCO to work with as care is coordinated through the enrollee’s team at the MCO.
Wisconsin has four MCOs. When an MCO plays such an important part in a person’s life, choosing the right one becomes essential. How can anyone compare such large and varied organizations? MetaStar helps maintain program standards and contributes data to user-friendly scorecards for each MCO. Potential enrollees can easily compare options and select the most suitable one based on impartial data that has been collected and reviewed by MetaStar.
MCO Scorecards—MetaStar Makes the Difference with Data
MetaStar’s Quality Compliance Review team conducts reviews annually to gather data for the MCO scorecards. The team reviews each MCO in the state. “It’s a comprehensive system-level evaluation to determine that they are meeting requirements and hopefully exceeding them,” said Alicia Stensberg, project manager for the External Quality Review Department at MetaStar. Data for the scorecard comes from program enrollee surveys, an extensive document review, and employee interviews, with the latter two completed by MetaStar’s team.
The MetaStar team reviews documents such as policies and procedures, monitoring data, training information, contracts, correspondence, and much, much more to ensure these documents meet the metrics set by the state and federal governments. Employee interviews conducted over two or three days, involving various groups of staff members—everyone from information technology to care team members to leadership to support and supervision staff gets interviewed. The interviews are done to corroborate the findings from document review, but Stensberg finds them interesting for another reason: “It’s neat to hear [the staff] talk about their passions for supporting members and helping people live full and safe lives. I hear about the different initiatives that they have and the ways that they’re being collaborative with different organizations and different resources, all in the name of supporting members. It’s a cool experience.” She cites an example of another state’s Medicaid program addressing gun violence, highlighting the importance of caring for enrollees’ needs beyond direct medical care. Stensberg continues: “If you’re looking at caring for the whole patient, gun violence is very, very real for so many of the Medicaid recipients. The amount of impact Medicaid has amazes me.”
Data from the review process helps reviewers identify a requirement as “met” or “not met.” If something is found to be deficient, Stensberg explains, the Wisconsin Department of Health Services (WI DHS) can implement a corrective action plan for the organization to make improvements.
The hundreds of pages of MetaStar’s technical review are distilled into key areas for MCOs, such as such as satisfaction, responsiveness, communication, care delivery, quality standard, staff turnover and staff ratios. The WI DHS compiles this data into easy-to-compare scorecards.
Additionally, the review data is reported to the Centers for Medicare & Medicaid Services (CMS) as an Annual Technical Report, which is hundreds of pages long (and available online for anyone who is interested.)
The MetaStar Quality Review Team
The Quality Reviewers are part of the MetaStar External Quality Review Department. Stensberg calls them “some of the most amazing people I’ve ever worked with. All of them are such strong advocates for the individuals receiving services and really understand how the systems operate.” They all have 10 years or more of experience in LTC or a related field, such as nursing, counseling, social work; they’ve worked with children’s programs and family care organizations. Stensberg herself previously worked with adults with disabilities, and, like the rest of her team, she thinks it helps her in her current work. While she misses the job, “I’m glad to be here because I’m still part of the field. I think I’m having an impact on a broader scale.” This all-star team ensures regular assessment of the MCOs so participants can be assured that the scorecards are a carefully considered collaboration between WI DHS and caring, patient-focused MetaStar reviewers.
In addition to the MCO reviews and scorecards, the External Quality Review Department is involved with another HCBS-waiver program: Include, Respect, I Self-Direct (IRIS). This unique program allows enrollees to have more control over what care they receive, where they receive it, and when. Be sure to check in next month when we discuss the IRIS program and its formula for giving enrollees more influence in the direction of their healthcare as well as more choice and more independence.
May is the American Stroke Association’s (ASA) American Stroke Month. Often unrecognized and untreated, strokes can have devastating consequences:
- Each year, nearly 800,000 stroke patients join the 9.4 million adults (20 years old or older) in the United States who have had a stroke and are living with its effects. Of those 800,000 patients, over 160,000 will die.
- One American has a stroke every 40 seconds, and one American dies of a stroke every 3.25 minutes.
- 40% of strokes in the United States occur in males, and 60% occur in females.
- The risk of having a first stroke is nearly twice as high for non-Hispanic Black adults as for White adults. Non-Hispanic Black adults and Pacific Islander adults have the highest rates of death due to stroke.
- Strokes rank fifth among all causes of death in the United States.
- In 2020 (the latest year for which data is available), 2,091 people in Wisconsin died of strokes.
• Strokes are the leading cause of disability in Wisconsin.
• About 25% of people who recover from their first stroke will have another one within five years.
• Up to 80% of strokes are preventable.
(Sources: Wisconsin Environment Public Health Tracking Program, The Centers for Disease Control and Prevention, Wisconsin Department of Health Services Coverdell Program, Stroke Awareness Foundation)
The cost of strokes in human lives and resources continues to grow each year. There’s no better way to mark this important awareness month than to discover the ways the Wisconsin Department of Health Services (WI DHS) and MetaStar are enhancing the continuum of care for stroke patients across the state.
The Quest for Better Stroke Care
Paul Coverdell was a Georgia Senator who died from an intracerebral hemorrhage in July 2000 while serving in Congress. He served the people of Georgia for nearly 17 years before his death at age 61.
This tragedy led to the creation of a new stroke care program. In 2004, the Centers for Disease Control and Prevention (CDC) established the Paul Coverdell National Acute Stroke Program in response to Senator Coverdell’s death and a three-year study on stroke care in the United States. The program provides funding to state health departments that are committed to improving stroke care.
Wisconsin’s community-based organizations, emergency medical services (EMS), hospitals, professional organizations (like the ASA and the American Heart Association [AHA]), academic institutions, public health, and industry partners work together to “ensure that all patients in Wisconsin receive timely, high-quality acute stroke care” (WI DHS).
MetaStar Meets Coverdell
Dot Bluma, BSN, RN, CPHQ, is MetaStar’s stroke project specialist. She provides invaluable support to the program. Bluma currently works with hospitals to analyze data, finding areas where more focus or education is needed. “I’m our data geek on this program,” she said with a laugh. “I’m a nurse, but I’ve become a data nerd.” She has three colleagues on the Coverdell team, one who works with EMS, and two others who work with community partners, all with the same goal of improving stroke care in Wisconsin.
Wisconsin Coverdell in Action
Though the broad focus of a Coverdell program is decided by the CDC, the awardee states can choose to work on specific areas anywhere along the stroke-care continuum that fit within the broader focus. Wisconsin has chosen several areas to focus on for the current program’s focus on disparities.
 “We always start with educating the community,” said Bluma. “How can we prevent a stroke from happening?” Educational materials created by the Coverdell team addressed that question. “Risk Factor Rick,” created in 2023, explains stroke risks and how to combat them. “BE FAST Bella,” created in 2017, educates about the signs of a stroke, using an acronym adapted from the ASA’s FAST acronym. With the most recent Coverdell program, the materials were translated into Spanish, Hmong, Somali, and Russian, which, along with English, are the languages most frequently spoken by stroke patients in Wisconsin. “We want to meet people where they are and be cognizant of everybody’s diversity,” Bluma said.
“We always start with educating the community,” said Bluma. “How can we prevent a stroke from happening?” Educational materials created by the Coverdell team addressed that question. “Risk Factor Rick,” created in 2023, explains stroke risks and how to combat them. “BE FAST Bella,” created in 2017, educates about the signs of a stroke, using an acronym adapted from the ASA’s FAST acronym. With the most recent Coverdell program, the materials were translated into Spanish, Hmong, Somali, and Russian, which, along with English, are the languages most frequently spoken by stroke patients in Wisconsin. “We want to meet people where they are and be cognizant of everybody’s diversity,” Bluma said.
Equally important is ensuring that when the patient goes home, their individual needs are met. In addition to medication, regular blood tests, and follow-up appointments, the Coverdell program provided the opportunity to begin including community resources in stroke recovery. Bluma described an integrated health program between the Milwaukee Fire Department (MFD) and Froedtert Hospital that refers certain high-risk stroke patients to the MFD Mobile Integrated Health Program (MIH). MFD performs home visits, assesses and addresses safety concerns, provides education, and more. MIH then sends a report back to Froedtert who enters the information into the database so outcomes can be studied. “It’s been a phenomenal connection,” Bluma said. ” Clients say it’s been worth its weight in gold.”
Decoding Coverdell Data
With so many areas that could be the focus of this much-needed program, how does Coverdell identify which areas should and could be targeted for improvement? They use data from the AHA’s Get With The Guidelines®-Stroke database. According to the registry, over 9.5 million patient records from over 3,400 hospitals have been entered. The database provides a rich data set for analyzing stroke care at the hospital, Wisconsin, and national levels. Factors like bed size, hospital certification, sex, and more can be analyzed and interpreted to improve the quality of stroke care. Bluma spends part of her time working in the database and helping hospitals with their data. EMS data can also be integrated into the Get With The Guidelines®-Stroke database to provide a fuller picture of patient care and transitions.
Additionally, Coverdell creates hospital report cards based on the Get With The Guidelines®-Stroke database. Hospitals can now easily compare their data and benchmarks with all Coverdell hospitals in Wisconsin and hospitals nationally. Similar report cards have been created for EMS as well.
The Future of Stroke Care
Bluma isn’t one to rest on her laurels. She continues to sift through data to identify ways to improve stroke care in Wisconsin. “Addressing disparities in stroke care is an area we need to have a bigger focus on,” explained Bluma. Through continued work by implementing evidence-based stroke care education and protocols to reduce geographic, racial, and ethnic disparities, MetaStar aims to pave the way for targeted approaches that address individual patient needs. Continuing to leverage the relationships between community-based organizations, emergency medical services, hospitals, and patients and families are crucial in successful pre and post stroke care. The ongoing approach is to continue to build on prior work, provide equitable and inclusive care to diverse communities, and leverage data and technology, to ensure the future of stroke care will be more equitable and effective.
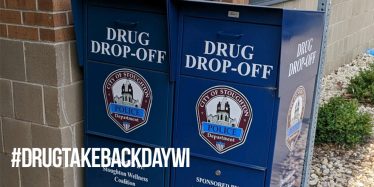 In the ongoing battle against the opioid epidemic, National Drug Take Back Day stands as a beacon of hope, fostering community engagement, and promoting responsible disposal of prescription drugs. This biannual event, held across the United States, serves as a vital initiative in combating the opioid epidemic and ensuring the safety of our communities.
In the ongoing battle against the opioid epidemic, National Drug Take Back Day stands as a beacon of hope, fostering community engagement, and promoting responsible disposal of prescription drugs. This biannual event, held across the United States, serves as a vital initiative in combating the opioid epidemic and ensuring the safety of our communities.
How National Drug Take Back Day Started
The inception of National Drug Take Back Day is resultant of Drug Enforcement Administration’s (DEA) realization of the pressing need for proper disposal of prescription medications.
Recognizing unused prescription drugs as hazards, the DEA, in collaboration with community members and other partners, launched the first Prescription Drug Take Back Day in September 2010.
Since its start, this initiative has garnered widespread support and participation from individuals, pharmacies, law enforcement agencies, and community organizations. The event’s success hinges on its simple yet impactful premise: to provide a safe, convenient, and anonymous method for individuals to dispose of unwanted prescription drugs.
A Biannual Event
National Drug Take Back Day typically occurs twice a year, in the spring and fall, with designated collection sites nationwide. (The next event is set for April 27, 2024.) These sites are often located in pharmacies, police stations, and community centers. The drugs collected are securely transported and incinerated, ensuring they do not end up in the wrong hands or harm the environment.
Participation in National Drug Take Back Day is crucial in addressing the multifaceted challenges posed by prescription drug misuse. By removing unused medications from homes, individuals reduce the likelihood of accidental ingestion, diversion to non-prescribed users, and environmental contamination through improper disposal methods like flushing down the toilet or throwing them in the trash.
Wisconsin’s Leadership in Take Back Efforts
Among the states leading the charge in drug take back efforts, Wisconsin has emerged as a trailblazer. Through strategic partnerships between state agencies, law enforcement, healthcare providers, and community organizations, Wisconsin has established a robust infrastructure for prescription drug disposal and education.
One key factor contributing to Wisconsin’s success is its extensive network of disposal sites. The state boasts a diverse array of collection locations, providing widespread access for residents across urban and rural areas.
Wisconsin community members have also implemented innovative ways to raise awareness and promote participation in drug take back programs. Public awareness campaigns, educational workshops, and outreach events are organized to educate residents on the importance of safe medication disposal and the risks associated with prescription drug misuse.
By fostering partnerships and leveraging resources, Wisconsin maximizes the impact of its drug take back initiatives and creates a united front against the opioid epidemic.
National Drug Take Back Day demonstrates the joint effort to protect communities from prescription misuse. For over a decade, it has made progress in promoting safe medication disposal. Do your part, access the Wisconsin Department of Health’s Dose of Reality: Drug Take Back Day page to find a local drop off location near you.