 On the Mission page of the Utilization Review Accreditation Commission (URAC) website, President and CEO, Shawn Griffin, MD, declares “At URAC, we seek to inspire health organizations and communities to deliver a higher level of care.” The page goes on to say that URAC knows “equity and inclusion can be improved. It’s our intention to continually define and write standards that elevate health care for each individual. Every person matters. Every person deserves the best care.” Figuring out how to get to that higher level of care can be a complex and challenging endeavor for most healthcare organizations. That’s why, in 1990, the newly incorporated URAC created standards and metrics that allow organizations to receive URAC accreditation. The accreditation shows that, through careful data collection and validation, an organization has reached an elevated level of healthcare delivery. Today, URAC offers dozens of accreditation programs to help healthcare organizations provide the best, most efficient health care at the lowest cost.
On the Mission page of the Utilization Review Accreditation Commission (URAC) website, President and CEO, Shawn Griffin, MD, declares “At URAC, we seek to inspire health organizations and communities to deliver a higher level of care.” The page goes on to say that URAC knows “equity and inclusion can be improved. It’s our intention to continually define and write standards that elevate health care for each individual. Every person matters. Every person deserves the best care.” Figuring out how to get to that higher level of care can be a complex and challenging endeavor for most healthcare organizations. That’s why, in 1990, the newly incorporated URAC created standards and metrics that allow organizations to receive URAC accreditation. The accreditation shows that, through careful data collection and validation, an organization has reached an elevated level of healthcare delivery. Today, URAC offers dozens of accreditation programs to help healthcare organizations provide the best, most efficient health care at the lowest cost.
Steps to URAC Accreditation
URAC accreditation is a multi-step process of data collection and validation. In healthcare, where it’s difficult to consistently measure outcomes between and within organizations, having a third-party organization—like URAC—allows healthcare providers and administrators to see how their organizations are performing using a set of predetermined metrics. Like the shiny gold star atop a school test, the URAC accreditation gold star lets everyone who sees it know that this organization has met the high standards set by URAC’s various panels of experts.
Accreditation happens in three steps: first, the organization applies to URAC to be accredited. For the remainder of that year, the organization reviews the required metrics for their area and adjusts their workflows, data tracking, and data storage systems to ensure they are tracking and collecting the required data. Next, the organization collects data for an entire calendar year for all mandatory metrics. The final step includes data validation by a URAC-approved validating organization such as MetaStar and the submission of that data to URAC. For example: if an organization applies to URAC in 2024, they collect their first year of data in 2025, and they would have their data validated for URAC submission in 2026. Data submission is required each year the organization wishes to be URAC-accredited.
Each URAC accreditation program has mandatory metrics used to evaluate their organizations. For example, mail service pharmacies will report on their prescription dispensing accuracy, such as the number of labels with incorrect patient addresses. This will be reported as a numerator (number of prescription labels with incorrect addresses) and a denominator (total number of prescriptions) to create a percentage of prescriptions with incorrect addresses. Measurement rates can then be assessed to find areas of improvement or areas of exceptional competence.
The Data Validation Process
During the validation process, MetaStar helps “confirm that the pharmacies/organizations are collecting the appropriate data and calculating the measure rates correctly,” said Ross Gatzke, the URAC data validation lead at MetaStar, during a recent interview. This means providing the organization with documentation to help them through the validation process, confirming they are collecting the correct data, and ensuring the organization is ready to report the required information to URAC. “For most of the mandatory measures that URAC has, organizations typically already have a data collection process in place,” Gatzke continued. “A lot of times, they just have to make some updates to meet the technical specifications [set by URAC.]”
MetaStar provides top-tier data validation services for pharmacies, which are the only organizations that require data validation for URAC accreditation. MetaStar validators continuously review submitted data and measure rates through the validation process. “It helps the organization feel at ease and get confirmation that they are reporting the measures accurately to URAC,” Gatzke explained. If any issues are found, the organization has time to adjust and run more data checks to ensure the final submission to URAC accurately portrays what happens at their organization.
The MetaStar Difference
MetaStar is one of the five URAC-approved data validation vendors. When deciding which vendor to choose, consider the following:
- MetaStar’s three-year retention rate (2022-2024) is 98.73%.
- MetaStar has the experience and consistency that organizations who are serious about URAC accreditation look for:
- Ten unique data validators. Each data validator has at least two years of experience, while most have five or more years of data validation experience. “They are subject matter experts in their own rights,” Gatzke said.
- A consistent, reliable relationship between MetaStar data validators and organizations.
- Year over year, the same validator will work with an organization, building a relationship on familiarity, trust, and knowledge.
- In subsequent years, data validation becomes a familiar process as the data validator will have experience and expertise working with the specific organization.
- MetaStar hosts three webinars twice each year that provide education and guidance regarding URAC data validation.
- MetaStar has outstanding customer service, and their data validators are among the best in the business.
Organizations praise MetaStar’s work, data validators, and customer service. Here’s what they say:
- [MetaStar is] dependable, quick to respond and extremely helpful. Everyone has been amazing and very friendly.
- The experience with MetaStar and our current reviewer is excellent. We have been customers for 5 years, and we enjoy the bi-directional learning that comes along with these audits and reviews.
- Our overall experience with MetaStar was excellent; our validator was very easy to work with and was very helpful every step of the way.
- We have been working with MetaStar for several years and continue to appreciate the quality and efficiency shown during the validation and reporting process!
- [MetaStar is] extremely professional and diligent. Working with our validator was a very positive experience where any question or concern we had was met with professional insight and remediation.
- Overall experience was fantastic. [MetaStar data validators are] extremely knowledgeable and helpful throughout the process.
If your organization wants top-of-the-line URAC data validation from a leader in the industry with proven, positive results, MetaStar URAC data validation services is the obvious choice. Contact Manny Martin, Vice President of Commercial Services at MetaStar, at 608-441-8264 or mmartin@metastar.com for more information or to get the contracting process started today.
WASHINGTON, D.C. (February 22, 2024) — The Leapfrog Group, a nonprofit watchdog organization that serves as a voice for health care consumers and purchasers, announced the return of On-Site Data Verification for hospitals and ambulatory surgery centers in 2024 with new partner MetaStar, a nonprofit organization with a wide breadth of experience in external quality review, healthcare quality consulting, and performance measurement.
On-site data verification builds on Leapfrog’s robust protocols for verifying Survey responses submitted via the Leapfrog Hospital and Ambulatory Surgery Center (ASC) Surveys. Hospitals and ASCs that participated in the 2023 Surveys will be eligible for On-Site Data Verification in 2024. Facilities selected for On-site Data Verification will be contacted by MetaStar in June 2024, and scheduled half-day visits will take place in September and October 2024.
Leapfrog hospital and ambulatory surgery center ratings are publicly reported on Leapfrog’s website and used by purchasers and consumers, regional and national health plans, transparency vendors, and researchers to identify the safest, highest quality facilities. The accuracy of the data we publish and distribute is of utmost importance. Leapfrog conducts extensive data review and verification, beginning with administrator attestations and an automated review of responses, to broad monthly response reviews and requests for documentation. On-site verification is one additional layer of quality assurance for a selection of hospitals and ambulatory surgery centers.
“We’re very excited to partner with MetaStar for on-site data verification. They bring a unique combination of unparalleled experience in quality review and performance measurement along with deep health care expertise across both hospitals and ASCs,” said Missy Danforth, Leapfrog’s senior vice president of health care ratings.
MetaStar has performed data review for a variety of other national organizations over the last 50 years and brings valuable expertise in developing verification processes and protocols to ensure that scheduled half-day visits are valuable and efficient for all participants. They have a long history of supporting hospitals and ASCs in collecting and reporting accurate data on a variety of patient safety and quality measures to various state, regional, and federal entities.
About The Leapfrog Group
Founded in 2000 by large employers and other purchasers, The Leapfrog Group is a national nonprofit organization driving a movement for giant leaps for patient safety. The flagship Leapfrog Hospital Survey and new Leapfrog Ambulatory Surgery Center (ASC) Survey collect and transparently report hospital and ASC performance, empowering purchasers to find the highest-value care and giving consumers the lifesaving information they need to make informed decisions. The Leapfrog Hospital Safety Grade, Leapfrog’s other main initiative, assigns letter grades to hospitals based on their record of patient safety, helping consumers protect themselves and their families from errors, injuries, accidents, and infections. For more, follow us on Twitter, Facebook, LinkedIn, and Instagram and sign up for our newsletter.
About MetaStar
MetaStar is an independent, nonprofit quality improvement organization with more than 50 years of experience, dedicated to effecting positive change in health and health care to achieve optimal health for all. Engaging with government agencies, health plans, and various stakeholders, MetaStar delivers a comprehensive range of services tailored to the unique needs of communities, payers, and healthcare organizations. MetaStar achieves impact by combining our long-standing reputation as a trusted advisor with evidence-based practices to drive improvement and accountability for quality healthcare.
Media Contact:
Susan Seidl
Marketing and Communications Manager
MetaStar
MetaStar has a grant from the Health Resources and Services Administration, or HRSA, to work with a coalition in Sauk County to reduce opioid overdoses. As part of MetaStar’s grant funding, the team worked with a local agency to create a position for a jail re-entry coordinator. This position was created because for people with substance use disorder, one of the times that is considered high risk for overdose is immediately after leaving jail. The re-entry coordinator meets with people while they are in jail and connects them to treatment and other supportive services, to help reduce the risk of overdose after release.
One re-entry coordinator shared this story:
Frank, a program participant, was interested in support for the sobriety he found while in jail. He also needed housing. The re-entry coordinator connected him with The Harbor Recovery Center in Portage for peer and group support.
Frank and the re-entry coordinator worked together to complete a prescreen for a housing program. He was given his former employer’s contact information and wrote them a letter inquiring about employment after release. He was also given information on how to renew his certifications for work and how to activate his FoodShare card.
Before his release, Frank spoke about how he felt like everything was coming together for him to be successful. On his first day out of jail, Frank went to the housing program office to meet the staff, moved into his temporary living placement, got his FoodShare activated, and started working with his previous employer that same afternoon.
After being released for less than three weeks, Frank was accepted into the housing program, which can provide up to 12 months of rental assistance and/or security deposit assistance. He continues working and receiving services to support his recovery from substance use disorder through The Harbor Recovery Center.
As of October 2023, the jail re-entry coordinator has served 128 individuals like Frank.
Grant # GA1RH42910
Program #: HRSA-21-088; CFDA 93.912
Award: $1,000,000 (over three years) 9/1/21 through 8/31/24
Project: HRSA Rural Communities Opioid Response Program (RCORP) Implementation Grant
Grantee/Applicant: MetaStar, Inc.
Supporting: Sauk County Continuum of Care Consortium (S4C)
Focus County: Sauk
Period of Performance: 9/1/2021 through 8/31/2024 (36 mos.)
2023 marked MetaStar’s 50th anniversary, a significant milestone that we celebrated with gratitude and a commitment to giving back. As we reflect on five decades of pursuing our vision of optimal health for all, our dedication to the well-being of our communities takes center stage. This anniversary year has been more than a celebration – it’s been a year of meaningful contributions. Throughout the year, our team members gave back in a variety of ways.
Virtual Blood Drive with the American Red Cross
We partnered with the American Red Cross for a virtual blood drive. Aligning with our anniversary theme, our goal was to recruit and secure 50 donors. We’re thrilled to announce that we exceeded this goal! These donations help ensure a crucial supply of life-saving blood is available for community members in need.
Fall Donation Drive Supporting United Way and Community Shares
In the spirit of the season of giving, we organized a fall donation drive for United Way of Dane County and Community Shares of Wisconsin. The entire MetaStar team heard directly from individuals from Safe Communities of Madison and Dane County (supported by the United Way) and Disability Rights Wisconsin (supported by Community Shares) and learned about the important work both groups are doing to support our communities and help them thrive.
Empowering Team Members to Volunteer
As part of our commitment to community engagement, MetaStar empowered our team members to contribute their time through volunteer opportunities in their own communities. Our team rose to this opportunity by providing over 100 volunteer hours to support mission-aligned organizations. Below is a list of some of the organizations our team supported in 2023:
- Madison Street Medicine in Madison
- Ronald McDonald House Charities in Madison
- Safe Shelter in Green Bay
- Kinship Community Food Center in Milwaukee
- Second Harvest Food Bank in Madison
- SOAR Fox Cities in Appleton
- The Stoughton Wellness Coalition in Stoughton
- H.E.L.P. (Help Excite Little People) in Sauk City
- Meals on Wheels in Madison
- Project Christmas of Jackson County in Black River Falls
- Allied Family Center Boys and Girls Club in Fitchburg
As we celebrate our 50-year legacy, we remain committed to “walking the talk” by giving back to the communities we serve – now and in the years to come.
How we can improve health equity with culturally and linguistically appropriate services (CLAS)
Everyone deserves quality healthcare services. CLAS standards can help tailor care to the patient’s unique needs and help them feel included in their care. If we all do our part, we can move health equity straight to the head of the CLAS!
The CDC defines health equity as “the state in which everyone has a fair and just opportunity to attain their highest level of health.”* Health equity is a tenant of high-quality care and should remain a commitment for the entire healthcare community, as outlined in the overarching goals of Healthy People 2030.
Dr. Kedar Mate, the Institute for Healthcare Improvement president and CEO, challenges that there can be no progress on quality without equity. And yet, our data continues to highlight the gaps in care by characteristics such as race, ethnicity, socio-economic status, and geography. Commitment exists to provide equitable care and reduce disparities across healthcare organizations, requiring changes in policies and practices. Guidance is available to help build such policies and procedures and assist with staff education to get us closer to providing culturally and linguistically appropriate services (CLAS).
CLAS sets forth standards and guidelines to help healthcare organizations deliver culturally aware care, encompassing many aspects of healthcare delivery, including communication, language assistance, and organizational culture. Health services that are respectful of and responsive to the health beliefs, practices, and needs of diverse patients can help understand and break down barriers to ultimately close the gap in health outcomes.
Bias Is a Barrier
While many healthcare professionals are well-intentioned and dedicated to offering high-quality care, explicit or conscious bias as well as implicit bias—an unconscious association, belief, or attitude toward any social group—can be a barrier for building trust with patients.
How might incorporating CLAS standards improve the implicit bias in the following examples leading to improved care?
- A doctor diagnoses a Black patient with diabetes and focuses initial treatment efforts on nutritional changes—without first exploring if nutrition is a central factor in the patient’s condition; making assumptions about what the patient is eating due to their race.
- A nurse practitioner is surprised when a Hmong patient seems hesitant to try a treatment plan, not knowing that the patient is afraid to say they want to first try traditional healing practices.
- A nursing home administrator assumes they are being inclusive by putting up LGBTQIA+ posters throughout the facility but does not consider talking to the residents who are members of the LGBTQ+ population about what would make their care and stay respectful and inclusive.
Sadly, bias too often leads to inferior care that is not personalized or equitable. Without incorporating CLAS, providers may miss opportunities to provide even better care for their patients. The CLAS standards are a blueprint of 15 standards for individuals and organizations, providing simple, effective ways to address health equity, improve quality, and eliminate disparities.
Breaking Down Barriers
- Be intentional and involve your intended audience. When creating CLAS materials, it’s important to both identify the needs of your intended audience and validate those needs by involving those most impacted in the development and design of services. For example, when creating materials for a Spanish-speaking audience, it’s not always enough to rely on a translation firm’s expertise. Instead, involve people whose native language is of the Spanish dialect for the patients being served. Ask them to help you understand nuances among differing dialects. This can go a long way in creating materials that help patients feel welcome, heard, and understood.
- Educate your staff. Healthcare providers earn trust by showing they are knowledgeable and empathetic. Incorporate training, across the organization, to build cultural competency and reduce explicit and implicit bias. Our reach extends beyond our internal employees. We’re proud to partner with the University of Wisconsin-Madison effort on Community-Academic Aging Research Network (CAARN), which brings together community and health system partners with academic researchers to conduct research to improve the health of older adults and decrease health disparities.
- Understanding, and using, Z-codes. Z codes, which are a category of ICD-10 codes, represent reasons for healthcare encounters that are not related to disease, injury, or external cause. Instead, Z codes describe social, economic, and environmental factors that influence a person’s health. These codes include issues related to education and literacy, housing and economic challenges, and difficult family circumstances. By using Z codes, instead of merely identifying a patient as having diabetes or other ailment, patient files alert the physician to potential problems that may be affecting the patient such as poverty, homelessness, food insecurity, or other personal challenges that can shape the physician-patient conversation. By having this information at hand, healthcare providers may better avoid biases and misconceptions that stand in the way of the most effective care. It allows the provider to have the necessary information to focus on the unique patient in front them.
Providing equitable care is essential to improving the health of the communities we serve. Through a commitment to the CLAS standards, we can support cultural humility across the continuum of healthcare and move closer to the ultimate goal of health equity for all.
*What is Health Equity? | Health Equity | CDC
September is National Recovery Month, an annual observance to educate Americans that appropriate treatment and mental health services can help those with substance use disorder (SUD) live healthier lives. Sadly, this ideal remains difficult to achieve because of bias in how we view addiction in this country.
At MetaStar, we’ve identified stigma as a primary major public health challenge. Stigma can prevent people with SUD from seeking help, even if they desperately want it. Educational programs and policy innovations have helped, but there is still work to be done to help eliminate stigma and help those struggling with SUD.
Systemic issues work against those fighting addiction
Imagine SUD as a very large boulder a patient carries with them every day. Should this person also have a mental health disorder—which often is the case—this adds a second boulder. If they happen to be a person of color, they’re weighed down by three boulders. If they’re a woman, by four, and if they’re living in poverty, five, and so on.
Despite good intentions, the healthcare community struggles with systemic issues in deploying appropriate, evidence-based treatment to those who most need it for SUD, as well as additional challenges. We know there are effective treatment options, but the question remains: How do we get the right treatment, to the right patient, at the right time?
Too often, the healthcare community chases the latest “solutions,” such as smartphone apps, telehealth, and AI-supported tools without reflecting on a root cause—stigma—and how overcoming that can help pave a smoother road to recovery.
Overcoming stigma
Stigma continues to cast a shadow over efforts to provide effective treatment for those grappling with SUD. This pervasive, societal shaming creates barriers at every stage of the recovery journey:
- Structural stigma leads to discriminatory policies and practices, such as a devaluing of treatment care providers, treatment entry procedures designed to present hurdles to those who are seeking care, and limited insurance coverage.
- Continued stigma on the part of healthcare providers can lead to mistreatment of those seeking help.
- And lastly, as people internalize negative stereotypes, it leads to feelings of shame and worthlessness, making a person feel as if they aren’t even worthy of getting better.
The Shine a Light podcast, which focuses on reducing stigma, recently featured a guest from a rural area who described her experience when seeking help. After finding herself at rock bottom, she made the brave decision to go to the hospital emergency department for help. After waiting for six hours, she received a curt response from the first doctor she saw: “I know what you’re here for, and I know what you’re all about. You’re not getting any drugs from me, so you should just leave.” This devastating experience kept her from seeking help again for a long time.
Shine a Light on Stigma
MetaStar’s two tenets related to the reduction of stigma are simple:
- Knowing, understanding, and empathizing with those with SUD helps defuse the negative impact of stigma.
- Words matter.
Not everyone has the opportunity or comfort level to get to know someone who has experienced SUD. Through our work with the Superior Health Quality Alliance’s Shine a Light on Stigma campaign, we’re able to bridge that gap. We offer informative, frank and action-oriented videos and podcasts to help people recognize their own prejudices and learn how to change them, humanize those struggling with SUD, and evolve the language we all use in discussing SUD.
Words matter. Using patient-friendly, person-centered language is a critical step in reducing stigma. For example, referring to “a person with substance abuse disorder” conveys an entirely different message and tone than labeling this same individual an “alcoholic,” “addict,” or “drug abuser.” The former suggests the person has a problem that can be addressed; the latter implies the person is the problem. By using person-centered language, you can show respect and kindness to people who may need it the most.
Take the pledge to reduce stigma
Because stigma is public health challenge, it requires community support to change it. That’s why we ask people and organizations to pledge to use appropriate, empathetic language and encourage others to do so, as well. We’re proud that people from across the nation have joined us, and the number continues to grow. We’ll continue our efforts throughout National Recovery Month and throughout the year, because changing stigma happens one conversation at a time.
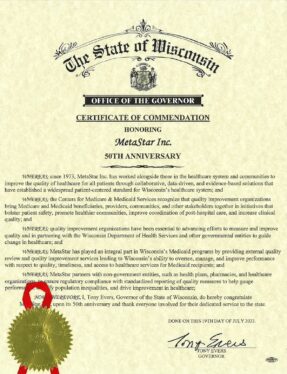
MetaStar recently received a 50th Anniversary Certificate of Commendation from Wisconsin Governor Tony Evers honoring MetaStar’s 50th anniversary. As an organization, we are proud of the work we’ve done to improve healthcare quality in the state of Wisconsin and beyond over the past five decades. We look forward to continuing to effect positive change in healthcare and patient safety well into the future.

Jesi Wang
By: Jesi Wang, MetaStar President & CEO
MetaStar is celebrating 50 years of dedication, partnership, and progress in effecting positive change in health and healthcare. We enthusiastically look forward to a new era in healthcare quality and patient safety, while recognizing our journey toward optimal health for all is ongoing.
In 1999, the Institute of Medicine (now the National Academy of Medicine) released a landmark report: To Err is Human: Building a Safer Health System. It shed light on a sobering reality: Preventable medical errors were contributing to tens of thousands of deaths in the U.S. each year.
The research called out staggering systemic failings, including fractured communication, inadequate training, and a lack of standardization in medical practices. Further, it pointed to a need to fashion a “culture of safety” based on transparency, the ability to report errors without fear of retribution, and, perhaps most important, learning from mistakes.
Since that report, significant improvements have occurred, thanks to the dedication of healthcare organizations and professionals. This includes the widespread adoption of electronic health records (EHRs); improvements in medication safety; implementation of learning systems and error reporting; fostering cultures of safety; and advances in telemedicine and remote patient monitoring. Yet there is more to be done.
As we look to the future of quality and patient safety, six key opportunities exist to further effect change and improve the lives of the individuals and communities we serve:
1. Better engage patients as true partners.
We need to prioritize active engagement in decision-making, while fostering collaborative relationships between healthcare providers and patients, to ensure care is tailored to individual needs and preferences for improved health outcomes and overall well-being.
A best practice example is the Moving Forward Coalition, a trailblazing group of more than 120 individuals and organizations focused on nursing home reform that routinely calls on groups of nursing home residents to identify problems and propose solutions.
2. Harness the power of clinical data to improve decision-making and health outcomes.
Emphasizing interoperability between healthcare providers and communities will facilitate seamless exchange of information, enabling comprehensive patient profiles and a holistic approach to care. We must acquire better data rather than just more data to advance patient outcomes and introduce efficiencies in healthcare processes. We need to think creatively about better ways to analyze, gather, share, present, and use data so the focus is on improved healthcare outcomes and not only data capture and measurement.
There are solutions such as the Wisconsin Statewide Health Information Network’s (WISHIN) Pulse, a patient-centric, longitudinal community health record that enhances clinical decision-making and empowers community providers to communicate, collaborate, coordinate, and provide whole-person care. WISHIN can help remove health information exchange or access-related barriers and impact health outcomes at both the individual and community levels.
3. Address health equity and the social factors influencing health.
By implementing targeted interventions that address disparities in access to healthcare, education, housing, and nutrition, we can address the broader system that shapes an individual’s health. Promoting policy changes and community-based initiatives that enable all individuals to achieve optimal health outcomes regardless of social circumstances is critical.
While studying substance use mortality in Dane County, the MetaStar team uncovered a stunning disparity between African American and White residents. While deaths occurred at a rate of 26 per 100,000 among Whites, Blacks faced mortality rates at nearly four times that level (96 per 100,000). Armed with this data, MetaStar met with individuals with lived experience to understand systemic gaps while designing cohesive and comprehensive large-scale improvement strategies. MetaStar will continue to braid wisdom with those most affected to amplify their voices and identify collaborative solutions.
4. Facilitate collaborative care and comprehensive coordination.
We will focus on addressing individuals’ holistic needs by designing, implementing, and evaluating programs that seamlessly coordinate healthcare providers with other settings of support, such as community organizations. By fostering information exchange, collaborative planning, and aligned measurement, we can establish a patient-centered system to ensure care and support are not only accessible and coordinated but aligned with an individual’s preferences, meeting them where they are on their healthcare journey.
One way MetaStar is supporting this work is by partnering with Sauk County Partnership for Prevention to strengthen and expand substance use disorder/opioid use disorder prevention, treatment, and recovery services to enhance rural residents’ ability to access treatment and move toward recovery. Partners are working across the health system, public health, and community to address root causes and to face such issues head-on.
5. Better support for older adults.
With our current population trends, supporting and empowering older adults will be critical to patient safety and healthcare quality improvement. With the expansion of home and community-based services (HCBS) efforts, older adults and people with disabilities will receive necessary assistance while remaining in their homes or living in community settings. This means new ways of thinking of quality in non-traditional settings, such as assisted living facilities and home-based care.
MetaStar continues to support long-term care facilities through assessment of quality standards, support with reporting needs, and creating a continuous quality improvement culture to help identify and address safety issues proactively, creating safer and more effective care environments for aging adults in all settings.
6. Amplify feedback, communication, and transparency.
MetaStar considers this, along with oversight and accountability, to be critical to a quality health system. Transparently sharing outcomes, safety data, and quality metrics not only fosters accountability but also builds trust among care settings and patients. By creating a culture that values open communication and learning from errors, healthcare providers can proactively address challenges, implement best practices, and consistently elevate the safety and quality of care. These initiatives ultimately result in improved health outcomes and patient satisfaction.
As an External Quality Review Organization and HEDIS Licensed Organization, MetaStar actively engages with healthcare providers, payers, beneficiaries, and stakeholders to gather valuable feedback that informs health and healthcare programs. Our commitment to feedback, communication, and transparency is evident in our comprehensive reporting, auditing, and validation services. Not only do these processes identify opportunities for improvement in health and healthcare, they also provide valid and reliable data that strengthens trust and guides effective decision making.
The familiar adage, “Rome wasn’t built in a day,” rings true as we consider the development of a flawless healthcare system. Just as it took time to shape the great city, achieving a near-perfect health system will take time. Still, progress made to date has been significant and highly encouraging, the outlook for the future is even brighter, and MetaStar stands poised to play a key leadership role in guiding positive change in health and healthcare. We are excited to collaborate with you in shaping this future.
Madison, Wis. – In July 2023, MetaStar, a leader in healthcare quality improvement, celebrates 50 years of promoting optimal health for all. MetaStar partners with government agencies, health plans, healthcare professionals, and communities to guide change in three key areas: healthcare quality consulting, external quality review, and performance measurement. For five decades, the organization has worked to effect positive change in health and healthcare and empower healthcare professionals, community organizations, and healthcare payers to make lasting improvements with a vision of optimal health for all. As part of the celebration, MetaStar has unveiled a new logo and website.
MetaStar, originally known as the Wisconsin Professional Peer Review Organization or WisPRO, was established following the US Congress legislation to review the necessity, appropriateness, and quality of medical care provided to Medicare beneficiaries.
In the 1990s, the team identified the opportunity to offer collaborative, technical assistance to health care organizations. The organization rebranded as MetaStar, meaning to “guide change.” Today, MetaStar’s scope has expanded to include quality assurance, quality improvement, community convening, and performance measurement.
MetaStar is led by Jesi Wang, MBA, who was named CEO in 2017. “I’m proud to celebrate 50 years of excellence, collaboration, and dedication to our mission. We have forged a strong legacy of leading health care quality improvement, and I look forward to the next fifty years of furthering our vision of optimal health for all.”
Today MetaStar partners with numerous hospitals, nursing homes, and communities on a variety of healthcare transformation, education, and performance management programs. Key areas of impact include:
- Advancing quality across the continuum of care to address topics such as substance use disorder, chronic conditions, and long-term care needs.
- Improving quality and compliance for Medicaid programs.
- Supporting HEDIS®, Initial Validation Audit (IVA), and other performance measurement programs to ensure accuracy of the data being reported.