
Photo credit: Hedi LaMarr
MetaStar fosters a positive and purposeful work culture to effect positive change in health and healthcare. The Culture and Wellness Committee guides programs, activities, and best practices to help create a supportive work environment for MetaStar employees.
Formation of the Culture and Wellness Committee
MetaStar has had a Wellness Committee for many years – working on programs, education, and opportunities to improve their health. When Human Resource Manager Susan Gunay joined MetaStar in 2020, she introduced the idea of integrating company culture into the existing Wellness Committee. The idea was supported, and the new Culture and Wellness Committee was formed.
The Wellness Committee members were invited to continue with the new committee and Gunay worked to recruit new volunteer members from across the organization, ensuring representation from each department.
Project Specialist Brent Amble shares, “Having the opportunity to be a voice and represent fellow employees is a privilege. By participating in the committee and sharing my opinion, I feel like I am contributing to the overall culture of MetaStar.”
Additionally, a charter was created to guide the committee. It includes the mission to discuss, plan, and manage organizational initiatives that promote a positive, fun, inclusive, and healthy work culture. An annual review of the charter and mission helps keep the group on track and aligned with MetaStar’s mission, vision, and values.
The committee meets monthly to work on employee appreciation, community-building activities, wellness initiatives, and other offerings to engage employees in the MetaStar culture.
Activities and Events
 The update to become the Culture and Wellness Committee occurred during the COVID-19 pandemic, which posed some unique challenges for the group. In December 2020, the group organized and hosted a virtual celebration to conclude the year. The committee bought snacks and treats, coordinated shipping to staff around the state and country, and ended with a virtual party featuring various breakout rooms and activities.
The update to become the Culture and Wellness Committee occurred during the COVID-19 pandemic, which posed some unique challenges for the group. In December 2020, the group organized and hosted a virtual celebration to conclude the year. The committee bought snacks and treats, coordinated shipping to staff around the state and country, and ended with a virtual party featuring various breakout rooms and activities.
“It was just a huge win because the committee needed to be creative and work hard to put it together,” recalls Gunay, “In the end, employees really enjoyed the virtual event and it helped to bring us all together during COVID, which was a tough time.”
Last summer, MetaStar hosted “Hay Day on the Midway” at the home office. The weather was beautiful, and the staff had a fun afternoon team building in person through food, outdoor games, and volunteer opportunities.
“It’s really all about the camaraderie and relationship building and having an opportunity to interact with leadership and work colleagues in person that help us establish and maintain our culture,” said Gunay.
Another major event organized by the committee is the annual end-of-year celebration. This is typically held offsite and includes food, activities, recognition, prizes, and plenty of time to mingle. “It’s a nice way for the organization to thank employees for all their efforts during the year,” explains Gunay.
Impact of Remote Work Opportunities
 After the pandemic, MetaStar studied how to best support staff in a new work environment while still ensuring we could continue to exceed our customer’s expectations. It was decided that staff could choose a remote, hybrid, or in-person work status if appropriate for their role. Ultimately, this change saved MetaStar resources, improved morale, and allowed us to provide more space for current and new tenants. However, the change caused MetaStar to look for opportunities for employee connection outside of regular meetings and spontaneous hallway conversations. It also gave the Culture and Wellness Committee additional challenges when planning events or programs. Organizing in-person events is a bit more complicated than it used to be. “It definitely affected how we thought about getting employees together and doing different activities,” Gunay explains, “We needed to think through the complexities of having many remote staff, whether it be the timing of events, so employees have sufficient travel time, coordinating with department level onsite meetings, etc. Many factors come into play. It is a lot of moving pieces.”
After the pandemic, MetaStar studied how to best support staff in a new work environment while still ensuring we could continue to exceed our customer’s expectations. It was decided that staff could choose a remote, hybrid, or in-person work status if appropriate for their role. Ultimately, this change saved MetaStar resources, improved morale, and allowed us to provide more space for current and new tenants. However, the change caused MetaStar to look for opportunities for employee connection outside of regular meetings and spontaneous hallway conversations. It also gave the Culture and Wellness Committee additional challenges when planning events or programs. Organizing in-person events is a bit more complicated than it used to be. “It definitely affected how we thought about getting employees together and doing different activities,” Gunay explains, “We needed to think through the complexities of having many remote staff, whether it be the timing of events, so employees have sufficient travel time, coordinating with department level onsite meetings, etc. Many factors come into play. It is a lot of moving pieces.”
Communication and Access to Resources
With staff utilizing remote, hybrid, and in-person work status, communication becomes critical to make sure information about events, programs, and opportunities is accessible to staff. Besides hosting a monthly All Staff meeting, MetaStar uses Microsoft Teams (Teams) and emails as well as MetaStar’s intranet as ways to share information.
The Culture and Wellness Committee has an information hub on the intranet, making things easily accessible to all staff, regardless of location. Each month, the committee contributes an article to the intranet for staff to access. The articles cover a range of topics on culture and wellness, such as mental health, specific health conditions, and exercise practices. Sometimes, they feature guest writers outside of the committee who may have a particular interest or subject matter expertise they would like to share with others. The committee also promotes events and resources available through MetaStar’s Employee Assistance Program.
New to the Culture and Wellness Committee’s efforts are the Employee Wellness Resource Groups. These are topic-specific Teams channels that staff can join to engage with other like-minded staff. Current offerings include:
- Mindfulness/Restore
- Movement and Exercise
- Nutrition/Food is Medicine
Volunteer employee facilitators share information, articles, and experiences. Staff can choose how much they want to participate, which helps increase engagement across the organization.
Looking Ahead
The committee’s current focus is to set dates for the summer and end-of-year events and brainstorm new ideas and themes. It is important to schedule event dates well in advance so staff can arrange travel and plan to attend.
The committee is also looking to increase engagement and participation in the existing Employee Wellness Resource Groups and perhaps start some new topics. The group continues to ensure the committee consists of volunteers who have the time and energy to contribute effectively and are a balanced representative of the departments and organization.
Everyone’s Efforts Impacts Work Culture
The work of MetaStar’s Culture and Wellness Committee plays an important role in fostering a supportive and positive work culture that reflects MetaStar’s values and mission. The committee’s impact on the culture comes through clearly when you look at the high level of retention and long tenure of employees. MetaStar has a retention rate of over 90%, with employees staying an average of nine years—more than double the national average of four years. Additionally, MetaStar achieved our highest staff engagement score in our history, 96%, in 2024.
Ross Gatzke, practice leader of URAC and IVA, explains, “The committee contributes to the positive work environment at MetaStar by doing much of the planning and logistics for company community building. These events (summer gathering, end of the year party) are important for staff morale and a great opportunity for engagement, especially as most staff are remote.”
Looking ahead, the Culture and Wellness Committee is committed to building on these efforts, continuously improving the workplace culture, and ensuring all employees feel valued, connected, and supported in both their personal and professional lives.
Making Health IT Easier for Behavioral Health Providers with Behavorial Health Connect
Navigating the complexities of health information technology (IT) can be challenging for everyone working in or receiving health care. Behavioral health providers and organizations face unique challenges related to electronic health record (EHR) implementation, privacy and security, data integration and interoperability, and funding. Starting in 2011, non-hospital-based physicians, some hospitals, and Medicare Advantage programs were eligible to receive assistance and incentive payments through the Centers for Medicare & Medicaid Services (CMS) EHR incentive programs. Behavioral Health providers were not eligible to participate in the CMS Incentive Programs. To bridge this gap, MetaStar offers the Behavioral Health (BH) Connect program, which helps providers use health IT to implement, optimize, and improve care.
The BH Connect program was designed based on the findings from a previous initiative that extended health IT technical assistance and training to Medicaid-enrolled behavioral health providers in Wisconsin. Twenty-nine organizations received assistance in the Behavioral Health Initiative (BHI) program which took place in 2020 and 2021. The BH Connect program builds upon the lessons learned from BHI and aims to outreach to over 200 BH providers that serve Medicaid members in the first two years of the project.
Covered Costs, No Cost to Practices
The BH Connect program provides support at no cost to the provider or organization, as it is covered by a contract with the Wisconsin Department of Health Services (DHS) Division of Medicaid Services. BH practices and organizations often cite cost and staffing challenges as barriers to EHR implementation or optimization. This program is a valuable opportunity for them to receive assistance at no cost. “It’s hard for providers to believe this assistance is available at no cost to them,” explains Mona Mathews, Program Manager of Healthcare Transformation at MetaStar. Behavioral Health providers and organizations who provide services to Medicaid-enrolled patients can join the program. An email to bhconnect@metastar.com will start the process and the health IT assessment.
Tailored Support – Choose Your Own “Adventure”
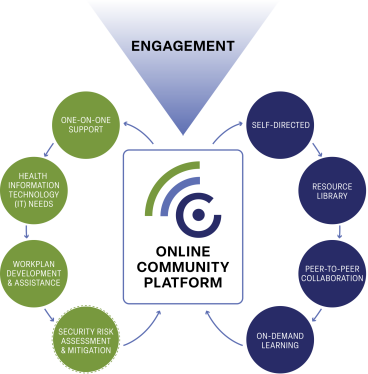
BH Connect provides participants access to customized support and assistance. Providers and organizations complete an initial assessment and access aligned resources independently through the BH Connect online community platform. One-on-one assistance with MetaStar project specialists is also provided where appropriate. Topics like security risk assessments (SRAs), health information exchange (HIE), data privacy, EHR selection, information blocking, etc., can be overwhelming. The MetaStar BH Connect team provides support tailored to the unique needs in behavioral health, guiding BH providers and organizations through complex challenges.
First Steps – Health IT Needs Assessment
Providers and organizations that join BH Connect complete a health IT needs assessment to evaluate how technology is currently used and identify specific needs such as EHR selection, and HIE, among others. A project specialist guides the process during a one-on-one meeting, or if an organization prefers, they can complete the assessment independently and follow up with a project specialist. Mathews said, “We set up time with them to walk through the questions and also provide some guidance.”
Personalized Attention, Multiple Areas of Expertise
The BH Connect team has a unique structure, featuring project specialist teams dedicated to two key areas of expertise: health IT and BH. “This team structure results in customized technical assistance and resources designed to meet the unique needs of behavioral health providers.” shares Mathews.
Custom Online Security Risk Assessment (SRA) Tool
MetaStar designed a custom online SRA tool that simplifies the annual process. The MetaStar SRA tool was developed based on guidelines from the Assistant Secretary for Technology Policy/Office of the National Coordinator for Health IT (ASTP/ONC).
Questions help MetaStar staff identify areas of risk associated with handling and safeguarding protected health information (PHI) including identifying threats and vulnerabilities that may affect the security of electronic PHI.
Mathews explains, “Using the ONC SRA information, MetaStar created simple yes and no questions.” The system allows the user to answer questions, flag questions, and return later to answers if more information is needed. Then, the system processes the responses and provides a risk mitigation plan.
“Every question also provides guidance,” Mathews continues, “You can click the guidance, and it explains the question in detail, including suggested documentation. In most cases, this step-by-step process can be guided by MetaStar project specialists. However, we are finding that those familiar with doing SRAs can complete much of the process on their own. Whether a provider requires one-on-one assistance or wants to do their own SRA using the MetaStar tool, there is no cost to the provider or organization.”
After the SRA is complete and a mitigation plan has been established, MetaStar’s project specialists provide active support to prioritize corrective actions the provider or organization can do to reduce the security risks identified in the SRA.
In some recent SRAs, MetaStar staff worked with participants on:
- Documenting processes by sharing sample policy and process documents.
- Identifying physical risks to patient health information by conducting facility walkthroughs.
- Providing privacy and security resources.
 BH Connect Online Community
BH Connect Online Community
The BH Connect online community is another no-cost resource available to participants. It provides a forum to connect with peers, download resources (including policy and procedure templates), real-time and on-demand education on topics such as 42 CRF Part 2, interoperability, EHR selection, and more. The platform connects providers and organizations and provides direct access to MetaStar’s project specialists.
Join BH Connect
The BH Connect program provides Wisconsin Medicaid-enrolled BH providers with a valuable opportunity to improve their health IT capabilities at no cost. In the first year of the project the BH Connect team has engaged with over 150 organizations to provide education, technical assistance, and resources to address their health IT needs. Privacy and Security and understanding interoperability are the top needs of participants receiving technical assistance. Since launching the online SRA application in November 2024, the BH Connect team has kicked off 13 SRAs. This no-cost SRA generates a final report that includes a Risk Mitigation work plan that allows organizations to address their risks and document their process.
From personalized expert support to comprehensive tools like the custom SRA Application and access to an engaging online community, BH Connect ensures you have the resources needed to improve care through health IT.
Don’t let the barriers of cost or complexity stop you from optimizing your practice; join the BH Connect program today. Reach out to us at bhconnect@metastar.com to begin your health IT assessment and unlock the full potential of your practice.
It’s a new year!

As we change our calendars to a new year, we find ourselves in a season of fresh beginnings and thoughtful resolutions. January is often a flurry of goal setting, New Year’s resolutions, and changes. However, MetaStar is already working to reaffirm our commitment to improving healthcare quality and outcomes. The Board of Directors wrapped up setting the organization’s direction in the last part of 2024.
MetaStar’s Board of Directors uses the Carver Model, a governance framework that emphasizes the board’s responsibility for defining “Ends”—the impact MetaStar exists to achieve—while delegating the means and operational responsibilities to organizational staff. The Board of Trustees reviewed MetaStar’s previous Ends and worked to revise and update them for 2025 and beyond.
MetaStar exists for systemic improvement in health outcomes, health care quality and safety and equity for communities and individuals across the continuum of care.
• System-wide transformation and improvement.
• Accountable and transparent systems.
• Reliable and trusted healthcare data.
• Collaborative impact.

Jesi Wang, MetaStar President and CEO
Jesi Wang, President and Chief Executive Officer (CEO), is rolling out the Ends to the organization in January. Then staff will develop the approach, determine what success looks like, how impact gets measured, and how it drives MetaStar’s impact priorities – advance behavioral health, expanding quality and home community care, and strengthening equity and quality.
The Next Iteration of MetaStar
To achieve these Ends, MetaStar incorporates a human-centered design process to define the approach to impact priority areas. “This is one of the strategic adjustments we are working on,” explains Wang, “instead of waiting for the government to set the priorities, we identify key health and healthcare gaps impacting the communities we serve, and work to drive meaningful change proactively.”
MetaStar is a very successful government partner and has a unique opportunity to drive local as well as national impact. “We won’t stop partnering with the government to drive health and healthcare improvement, that is who we are at our core,” said Wang. “However, if we see there are opportunities that aren’t being addressed, we will proactively engage government agencies and other funders to really drive improvements in those critical areas.”
By 2026, MetaStar plans to pilot and test the services and products developed to drive change as it relates to the established impact priorities.
Navigating Change with Experience
MetaStar’s decades of experience navigating administrative transitions position us to respond effectively to shifting federal priorities. “Every administration change brings new focus, new priorities, new opportunities, things we stop doing, and things we add,” shares Wang, “And I anticipate 2025 will be a year of shifting priorities. It does start off with some uncertainty of what the priorities and opportunities will be. However, both sides of the aisle see health care as an area for improvement.”
“We are good at being able to understand what the federal government’s priorities and needs are and translating those to what is most valuable at the local level,” explains Wang, “so that we can get things accomplished.”
Inspiration
Inspiration can serve as motivation for change. Wang is inspired by the MetaStar staff and the work they do every day to effect positive change. Recently she shared, “I have family member enrolled in the Family Care program, and hearing how well those programs are running for them inspires me. It also inspires me when I hear when programs or organizations are not running well, because I know [MetaStar] can make it better.” Wang is also inspired by the collaboration across the state, recently seen while working on a large proposal focused on Wisconsin’s unhealthy alcohol use.
“As we talked to individuals across the state, you could feel the passion they have for their work. I hear the same passion in our team, in healthcare workers, in healthcare organizations, and in the collaborators, we partner with,” said Wang, “That inspires me because I know if we can focus our efforts and align our priorities, real change can happen.”
Fast Forward – What Does a Successful 2025 Look Like?
Wang shares, “By December 2025, I hope we can confidently say we’ve made measurable progress in each of the four areas outlined in our Ends. I want MetaStar to be the first organization people think of when addressing gaps in care, quality, patient safety, or equity. When they face these challenges, I want them to say, ‘I’ll call MetaStar — they’ll help me figure this out.’ And we’ll get it done together. No single organization has all the answers, but by combining our expertise with the incredible talent across the state, we can truly make a meaningful impact.”
MetaStar works to improve health and healthcare, contact us to be part of the change in 2025.
Cue the fireworks! The talented teams at MetaStar are celebrating 2024: a year marked by excellence, teamwork, and unwavering dedication to improving healthcare quality. This year has been a testament to their mission to effect positive change in health and healthcare and to provide quality health for all. Below, some of the projects and collaborations from 2024 are showcased. These projects demonstrate the myriad ways MetaStar uses its unique position as Wisconsin’s largest independent healthcare quality organization to drive health care quality, safety, and equity outcomes. Looking ahead, they see even greater possibilities in the years to come.
Data-Driven Opportunities

Jesi Wang, MetaStar President and CEO
“The support MetaStar provides organizations and communities is a little bit like glue,” said Jesi Wang, President and Chief Executive Officer (CEO) of MetaStar. “When the glue is working well, you hardly notice it, but it holds everything together. When it’s not there, things have a hard time sticking.” This “glue” comes in the form of the various reviews, consulting, support, auditing, and more that MetaStar does to ensure quality healthcare for the residents of all 50 states.
One essential part of that work is external quality reviews. MetaStar has over 45 years of experience performing independent assessments, helping organizations meet and exceed the standards set by The Centers for Medicare & Medicaid Services (CMS). “We see it as an opportunity to shine a light on organizational and programmatic areas for growth and improvement,” Wang said. “That allows government agencies and healthcare organizations to focus on meaningful changes that strengthen quality and equity in care.”
External quality reviews play a key role in helping organizations and providers understand evolving standards and guidelines set by government or professional associations. In the video below, Vanessa Lamal and Lauren Mueller, two of MetaStar’s nurse reviewers, share their experience supporting organizations as they implement new guidelines from the American College of Obstetricians and Gynecologists, helping ensure providers are equipped to deliver high-quality care to mothers during the post-partum period.
Another example of how independent review and oversight drive quality is the significant improvement in care plans across seven Medicaid and Home and Community-Based Services (HCBS) programs—including Children’s Long-Term Support Program (CLTS), Family Care, Family Care-Partnership, Program for All-Inclusive Care for the Elderly (PACE), and Include, Respect, I Self-Direct (IRIS). The percentage of care plans documenting the strengths, preferences, and needs of members increased from 73.5% last year to 94.2% this year.
MetaStar also plays a critical role in supporting timely grievance and appeal investigations. As of November 11, 2024, 651 investigations were completed for the IRIS program, which empowers adults with disabilities and older adults in Wisconsin to make decisions about how they want to live their lives. MetaStar serves as a trusted third-party mediator, addressing issues between Medicaid recipients and service or support providers.
Collaborating for Improved Care
MetaStar focuses on improving healthcare quality in underserved and underrecognized areas. One of those areas is another topic in women’s health—urinary incontinence (UI), an uncomfortable topic for many. “We also work to effect change where there might be stigma or things folks don’t want to talk about,” Wang explained. “Urinary incontinence in women isn’t a provocative, sexy topic, but it has great impact on the lives of the individuals who suffer from it.”
In collaboration with University of Wisconsin-Madison’s School of Medicine and Public Health, the Medical College of Wisconsin, and the Agency for Healthcare Research & Quality, MetaStar successfully integrated screening guidelines for UI into medical practice. This enabled competent and caring discussion of the topic, breaking down the stigma surrounding it. One of MetaStar’s practice facilitators, Hannah Trickel, explains the way MetaStar relied on established relationships and collaboration with other organizations to advance quality for women in Wisconsin.
One of the strategic advantages of MetaStar is that “we really believe in collaborative solutions and collaborative impact,” said Wang. This collaborative partnership resulted in a significant improvement in women’s UI screening: it improved by an average of 47%, exceeding the original 20% goal.
Another example of MetaStar’s collaborative efforts to improve care and reduce stigma is its focus on advancing behavioral health, particularly addressing substance- and opioid-use disorders. As a partner organization of Superior Health Quality Alliance, MetaStar has played a key role in producing trainings, videos, and resources tailored for multiple care settings. One impactful initiative is the “Shine A Light On Stigma” campaign, which encourages organizations to pledge to eliminate stigmatizing language related to behavioral health and substance use. “By working together, we can create a more compassionate and supportive environment for all individuals,” Wang explained.
Ensuring Data Reliability
MetaStar’s certified auditors validate and certify data for programs such as HEDIS®, URAC, and more, ensuring accuracy and reliability in reporting. The MetaStar team ensures organizations meet rigorous standards and regulatory requirements, helping organizations maintain compliance, enhance data integrity, and drive quality improvement initiatives.
“We view ourselves as not just a vendor who’s going to check the boxes for [customers], but as someone who can help them solve problems,” said Wang. “It shows up in the way we do our work and the way that our staff partner with individuals and organizations.” Ross Gatzke, URAC and Initial Validation Audit (IVA) project lead at MetaStar, shares a challenging situation where they were asked to perform a URAC data audit in six weeks instead of the usual three or four months. Gatzke explains how MetaStar made it happen.
In 2024, MetaStar completed 311 performance measurement audits and supported 159 customers. This superior customer service leads to MetaStar’s high quality outcomes and customer satisfaction results Wang cites this ethos as one of the things she’s most proud of at MetaStar: “Everyone [at MetaStar] makes a commitment to show up, and they really believe in the work that we do. They believe in the impact we can have and take that extra step.”
Using the Past to Improve the Future
“The impact and progress in 2024 mark another year of success and valuable experience building quality infrastructure for organizations across the state and the country,” said Wang. While 2024 is projected to be MetaStar’s most successful year in the last decade, Wang is already looking ahead. MetaStar has already identified three critical impact priorities for 2025: continuing to advance behavioral health, expanding quality in home and community care, and strengthening equity and quality. One area of focus will be on unhealthy alcohol use. “Wisconsin continues to be a ‘leader’ of unhealthy alcohol use and behaviors,” Wang explained. Bringing together a wide range of collaborators, Wang is excited to “think about how holistically we could drive change across the state.”
As priorities evolve, Wang is confident MetaStar will remain a leader in healthcare quality improvement. With over 50 years of experience in this space, she believes MetaStar will continue to innovate and advocate for optimal health for all. “We have a deep history of doing this work, and that commitment isn’t going to change,” said Wang. “The organizations we partner with are doing tremendous work, and while there are many challenges, it is those challenges that drive us. We’re motivated by the opportunities for change, working every day to make healthcare better.”
In the highly competitive and vital industry of health care quality, MetaStar provides clients with a unique advantage: tailored software development solutions.
Their exceptional software development team is equipped to provide custom software solutions that meet a diverse range of customer needs. This commitment enriches customer experiences and solidifies MetaStar position as an industry-leading innovator.
Small Department, Big Wins
The MetaStar Department of Information Technology (IT)—a talented group currently comprised of four developers, an enterprise network administrator, and Director Karl Stebbins– has successfully crafted over 50 custom software programs. All are designed to help MetaStar’s customers, employees, and partners record, track, evaluate, and report on the gigabytes of data housed within MetaStar’s servers. New programs are launched while others are phased out, but all are meticulously designed and tested to ensure efficient task workflows and accurate reporting.
“MetaStar is unique because we’re small,and most organizations our size don’t typically engage in software development,” Stebbins said, “and we’ve been doing it for decades.”
Stebbins recalls that he inherited the software development team and their existing mainframe computer system when he started at MetaStar almost 30 years ago. MetaStar had only two clients at that time. Now, MetaStar has hundreds of clients in all 50 states who can access MetaStar’s software through web portals. All programs are created under the guidance of Stebbins by skilled developers, align with Health Insurance Portability and Accountability Act (HIPAA) standards where applicable, and in accordance with SOC 2® certification.
Data Collection Drives Reporting Development
MetaStar has existing software for the four types of data validation organizations it works with: URAC, Health Effectiveness and Data Information Set (HEDIS), and Medicare Parts C & D. Additionally, MetaStar gathers Initial Validation Audit (IVA) data. The IVA software is one of the biggest created by MetaStar and is regularly accessed by customers, coding vendors, developers, and MetaStar employees.
When collaborating with certifying and accrediting organizations, additional factors come into play. Many of these organizations update their specifications and requirements annually. In response, MetaStar’s team of developers diligently update, or “rev”, many of the software programs each year with the help of the programs’ auditors. “Developers are often pressed for time when it comes to understanding The Centers for Medicare & Medicaid (CMS) and National Committee for Quality Assurance (NCQA) rules, so we rely on the MetaStar auditors, who are already the experts, to guide us on the necessary changes,” Stebbins shared.
Ensuring the proper formatting of data or reports submitted for accreditation is another special concern. Data reporting is one of the largest uses of the MetaStar software, requiring the dedicated efforts of one full-time developer. “We have hundreds of reports that we produce,” Stebbins explained. “One application can generate a dozen of reports—management, summary, aggregate, statistical, tabular—all kinds of reports that go into varying levels of details.”
While some of these reports are for internal purposes, others are submitted to accrediting agencies, like URAC and HEDIS. Once all required data has been entered, the customer can then effortlessly export it in the appropriate file format. “Certain organizations prefer specific data file formats, while others require complete folders of documents. Each set of requirements is unique,” Stebbins said. Sometimes these requirements can be especially specific. Stebbins recalled a story of a customer being overwhelmingly particular about page numbering. “Page numbers are a decades-old issue,” he shared with a laugh. “That’s mostly for printing, and information isn’t consumed like that much anymore.”
Meeting Client Needs With Software Solutions
A lot of software program concepts come from clients approaching MetaStar with a specific need, and, as Stebbins stated, “we’ll tell them we can automate that with an application.” He emphasized: “Many customers are unaware they can request an application rather than relying on a manual process.” He credits MetaStar’s extensive and growing customer base for MetaStar’s ability to automate workflows that can be “highly tailored to the needs to the customer, the workflow, or the federal requirements.” Some examples include software for performing security risk assessments at behavioral health sites; an application that tracks obstetric data to help improve fetal mortality rates; and an application called No Wrong Door which measures return on investment for Aging and Disability Resource Centers (ADRCs) in Wisconsin.
“Customers find MetaStar’s experience building and adapting databases as well as their experience with reporting valuable,” explained Jenny Klink, MetaStar’s Vice President of External Quality Review. Klink cites feedback from the Medicaid Family Care, Partnership, and PACE Compliance and Quality Directors both praising the File Drop Zone program which allows them to upload quality compliance review documents. “Both were very pleased to move away from lengthy spreadsheets and file labeling processes,” Klink said.
MetaStar Employees Invent Software Ideas
Lastly, innovative sparks for software ideas and features are created by the MetaStar employees who use them. Alicia Stensberg, a project manager on the Long-Term Care team at MetaStar, identified an opportunity for enhancement in the Family Care Care Management Review (CMR) software. She requested a feature to automate the cumbersome process of manual notifications between reviewers and managers, streamlining communication. “Her idea turned into a standard workflow,” Stebbins said. “It allows them to do their job, do it efficiently, and do it with improved accuracy.” This feature has also been added to other programs in the last year.
Fast Action Lead To Stellar Support
While MetaStar doesn’t seek out customers for custom software development, they are glad to talk about possibilities that await prospective and customers “We can develop any software application, for any contract, and we can do it rapidly,” Stebbins said, proudly. He recounts a story of when the Wisconsin Department of Health Services (WI DHS) quickly needed a new partner for one of their software programs. MetaStar stepped in, saved the day, and still supports them.
“We can streamline projects because we’re narrowly focused. We perform one type of software development, and we use one set of technologies,” Stebbins explained. “It’s portable, it’s flexible, and we can deploy changes quickly.” Despite that narrow focus, the applications they create and the different workflows they can support are as varied and ingenious as the customers they serve.
Klink points to two recent noteworthy approaches in MetaStar’s custom software. First, external facing applications allows, “entities submitting documentation to upload it directly into the software used by the review team,” explained Klink. These documents are linked to the appropriate requirement, simplifying the process for reviewers to access submissions and record findings within the system.
Second, an internal application, the Medical Records Tracking System, allows team members to find a record and check its status at any time during the review process. The system is integrated, allowing team members quick access to the record through a unique record identifier for any of five separate review applications. The system can also be used for assigning records, identifying records for review, reporting, and billing. Klink echoes Stebbins’s sentiment that “MetaStar’s experience with building and adapting databases and reporting is why customers find our approach valuable.”
MetaStar Provides Innovative and Tailored Software
In a landscape where health care improvement companies often promise personalized attention and tools, MetaStar distinguishes itself by developing and delivering original and user-friendly software solutions suited to the needs of its customers. Their specialized, narrow focus, and dedicated team of developers can create monumental improvements in efficiency and accuracy. “[MetaStar’s IT team] is not trying to do everything. We’re focusing on what we do best,” Stebbins said. That has clearly guided them towards exceptional software and remarkable success.
“Health equity is the attainment of the highest level of health for all people. Achieving health equity requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and social determinants of health — and to eliminate disparities in health and health care.”
 The definition of health equity above comes from Healthy People 2030, a program from the US Office of Disease Prevention and Health Promotion. As it states, health equity and the forces that affect it extend beyond hospitals and clinics, and even beyond traditional medical centers, into communities, workplaces, and homes. It also applies to a setting many Americans might not think about often: nursing homes. With an aging population, a shortage of healthcare workers, and a struggling healthcare system, these microcosms face the unique challenge of providing quality medical care for their residents and a safe, comfortable, and dignified home. However, behind the stereotypes and media hype, people strive to create a medically competent and culturally responsive environment full of well-cared for residents.
The definition of health equity above comes from Healthy People 2030, a program from the US Office of Disease Prevention and Health Promotion. As it states, health equity and the forces that affect it extend beyond hospitals and clinics, and even beyond traditional medical centers, into communities, workplaces, and homes. It also applies to a setting many Americans might not think about often: nursing homes. With an aging population, a shortage of healthcare workers, and a struggling healthcare system, these microcosms face the unique challenge of providing quality medical care for their residents and a safe, comfortable, and dignified home. However, behind the stereotypes and media hype, people strive to create a medically competent and culturally responsive environment full of well-cared for residents.
Nursing Homes and Social Determinants of Health
“Nursing homes are people’s homes, so they are socially complex environments,” said Emily Nelson, MetaStar’s Vice President of Healthcare Transformation. “We need to recognize that the injustice of health disparities does not go away once someone begins their journey in a nursing home setting of care.” Many of those disparities can be attributed to social determinants of health (SDOH), which are “the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks,” according to the US Department of Health and Human Services. These SDOHs – such as educational background and opportunities, socioeconomic status, housing or lack thereof – significantly impact an individual’s health, functioning, and quality of life.
In nursing homes, “many of these SDOHs have already impacted individuals so greatly,” said Aimee Rasmussen, Nursing Home Program Manager at MetaStar. This presents a challenge to nursing homes—addressing these complexities requires time, understanding, education, and funding. However, she continued, it also presents an opportunity to address these areas of a resident’s ’s life by “providing a community and social environment that identifies these SDOH and takes action to resolve inequities.”
Privilege, Power, and Population Change
Nursing homes often face disparities in patient privilege and power which can lead to a decline in health equity. A 2024 Centers for Medicare and Medicaid Services (CMS) report revealed that in most post-acute care settings, Non-White patients had worse discharge to community and Medicare Spending Per Beneficiary outcomes than White patients, and outcomes worsened as the number of Non-White patients increased. Research also shows that Black, Indigenous, and people of color (BIPOC) experience a lower quality of life than White patients across various domains, such as food, relationships, and caregiving (Shippee et. al, 2022). Additionally, noted Rasmussen, there can be a struggle between short-term and long-term residents due to different goals and care needs.
The payors of nursing home residents can indirectly impact the care they receive, Rasmussen explained. “While residents residing in a nursing home receive the same care regardless of payor type, the organization itself may be impacted by the payor mix within the nursing home.” Private payors usually reimburse more than Medicare and Medicaid. High numbers of Medicare and Medicaid residents can lower reimbursement rates, negatively impacting staff, leadership, training, and resources. Race (or skin color) and payor status are just two of the many areas in which relative privilege and power affect the care and outcomes in a nursing home.
The makeup of nursing home populations is changing as well. A 2021 report from SAGE USA and the HRC Foundation estimates that 5% of people in long-term care communities identify as LGBTQ+. Other populations that were once a small portion of nursing home residents are growing as well, such as those with or who develop opioid use disorder or other substance use disorders; unhoused people who have nowhere to be discharged to; residents with increasing complex mental health needs; residents whose first language is not English, and more. As these minority identities accumulate, they become more ostracized and face more inequities (See Kimberlé Crenshaw’s theory of intersectionality.) These populations are stigmatized, and it can be difficult for staff and other residents to recognize the differences in privilege and power.
Staff language can also contribute to healthcare inequities in nursing homes. Terms like “addict” and “alcoholic” perpetuate the negative stereotypes of people who have substance use disorders. Terms like “the elderly” and “seniors” carry negative connotations for older adults, while referring to residents by their conditions, room number, or other features can be demeaning as well.
Differences in SDOHs, privilege, and power can significantly impact the health care provided to residents in nursing homes. For example, Rasmussen mentions that rashes, pressure injuries, and other skin issues look different on different skin tones, and staff members may not be adequately trained to handle these differences. Other populations may arrive with unfamiliar conditions and medications, requiring additional training.
Helping Nursing Homes Succeed
It is no secret that the nursing home industry faces challenges due to inequities, but organizations like MetaStar, Superior Health Quality Alliance, SAGE (which produces the Long-Term Care Equality Index with the HRC Foundation), CMS, and more are actively working to address these issues.
MetaStar collects data on nursing home outcomes and can “get in front of CMS to share what we’re seeing, hearing, and feeling in [the nursing home community] in a neutral fashion,” said Nelson. MetaStar, along with the Wisconsin Health Care Association and LeadingAge Wisconsin, trained over 2,300 licensed staff and 4,000 direct care staff in Wisconsin about assessing skin and wounds in people with a wide array of skin tones. Superior Health provides a resource library, including specific items about stigma, health disparities, and learning modules for frontline staff. Think Cultural Health, a website sponsored by the US Office of Minority Health, offers the Culturally and Linguistically Appropriate Services (CLAS) standards to help nursing homes create policies and healthcare that consider patients’ cultural and linguistic backgrounds.
There is also a lot that nursing home staff can do within their organization to help ease existing disparities. “Equitable care starts on or before admission,” Rasmussen said. “Providing the nursing home with a social history of the resident is key in this.” She emphasized the importance of knowing the resident’s story, whether it’s shared by the resident, their family, or both. This information helps staff understand who the resident is now and recognize the journey that brought them here. Rasmussen continued, “The more the nursing home staff know about the resident and their goals, preferences, and priorities, the easier it is for equitable care to be provided.”
Involving all staff in promoting health equity in nursing homes is crucial. Life enrichment staff can help identify special days or events for residents, and dietary staff can inquire about special foods or dietary needs. “These are important ways for the staff and residents to better understand and recognize cultural and religious beliefs of the residents they care for,” Nelson said. Nursing home leadership can ensure staff receive training on topics such as CLAS standards and promote an equitable culture across the organization. Policies and procedures should be written and implemented with health equity at the forefront, fostering a more inclusive environment.
Many people overlook the importance of nursing homes until they or a loved one needs to be cared for in one. “There is a lack of acknowledgment of the amazing work that is done in nursing homes in Wisconsin and beyond,” Nelson said. The complex challenges nursing homes face and their commitment to quality care are often overlooked. Despite this, nursing homes continue to find inclusive ways to create a diverse environment and unique community—with some help from outside sources. “MetaStar has long-standing expertise in health equity and nursing homes, creating a great opportunity to support nursing homes in their journey towards improvement,” said Nelson. “We are very confident that the skills, knowledge, and compassion are woven into the hearts of so many staff who have dedicated themselves to working in nursing homes.”
Medicare Parts C and D data validation for 2024 may seem far off in the future—it’s not even 2025 yet!
However, it will come sooner than expected, and it’s important to be ready rather than getting caught off guard. MetaStar offers top-notch audits and superior support during all phases of data validation. MetaStar’s exceptional net promoter score of 100 (out of 100) and impressive average customer recommendation score of 9.7 (out of 10) can be attributed to several reasons.
 Pre-audit Pre-planning
Pre-audit Pre-planning
Matt Walder, MetaStar’s data validation program lead, outlines the pre-audit preparation offered by MetaStar. This includes a webinar titled “Data Validation 101,” where clients learn about the fundamentals of the data validation project. Additionally, MetaStar hosts an all-client kickoff meeting to provide an overview of MetaStar’s data validation process and to share news and updates from the Centers for Medicaid & Medicare Services (CMS).
Following the all-client kickoff meeting, an individual call takes place between the MetaStar auditor and client “to answer any questions, to set expectations for the upcoming year, and get everyone on the same page,” explained Walder. After attending these meetings, clients have the necessary information to ensure a smooth and effective data validation audit.
Audit Assistance and Assurance
Once the data validation season begins on April 1, MetaStar auditors initiate the data validation audit, encompassing source code review, data recalculation, document collection, a virtual on-site visit, process review, and more. Throughout the process, MetaStar’s auditor maintains open communication with the client. They actively engage in dialogue, addressing inquiries, providing assistance, facilitating the exchange of necessary documents, and promptly responding to requests. “Our auditors guide you through every step and are always a resource throughout the year,” Walder said.
The success of MetaStar’s data validation program is in no small part due to the exceptional audit staff and the processes MetaStar has put in place. Walder stated that the audit team maintains continuity with clients year after year, fostering strong relationships and familiarity with processes and systems.
MetaStar auditors have been performing Parts C and D data validation since the program’s inception in 2011. In addition, all auditors are certified in Healthcare Effectiveness Data and Information Set (HEDIS) and have experience with URAC accreditation data validation, making them highly knowledgeable in healthcare plan data. “They have good relationships with their clients,” Walder said. “The auditors can get you through your first year successfully, and there’s a lot of collaboration along the way.”
Essentials Plus Extras
In addition to data validation, the auditors at MetaStar provide additional assistance to ensure a seamless audit process. “We’re in contact regularly throughout the year to answer any questions,” Walder said. MetaStar’s auditors are also clear and open during the audit process and in sharing the findings they uncover. “There should be no surprises. We try to be as transparent as possible,” Walder said, referring to the data validation scores. “We explain our findings to our clients, and make sure they are in agreement. We’re in contact throughout the season, and we follow up with any questions or additional documentation requests we may require.”
Auditors can also offer valuable insights into the data validation process. Walder encourages clients to ask their auditor about successful audit practices they’ve observed from other clients. These insights are shared anonymously. “We’re transparent and collaborative, and we want to see our clients succeed,” Walder said.
Walder also offers some helpful suggestions for a successful audit. “Choose your auditor early,” Walder advises. “We only have 10 weeks to get the audit finished.” With a wealth of experience and a proven track record of success, MetaStar’s data validation team stands out as the top choice for Medicare Parts C and D data validation. The auditors understand the complexities of the process and the importance of accuracy and reliable data.
Above all, MetaStar prioritizes its clients, as Walder explains, “From a process perspective, we do our best to ease the burden on [the client] because they have so many other priorities. We try to make their lives easier.”
For more information about MetaStar’s Medicare Data Validation program, contact Manny Martin, Vice President of Commercial Services, at 608-441-8264 or mmartin@metastar.com.
Last month, this blog discussed the managed care organization (MCO) scorecards created with review data collected by MetaStar. These scorecards enable enrollees in Wisconsin’s Home and Community-Based Services (HCBS) programs to easily compare MCOs and select one that has been fairly and impartially reviewed. There is another program that falls under Medicaid HCBS in Wisconsin: Include, Respect, I Self-Direct (IRIS). Since 2008, the IRIS program has operated as a self-directed program by the enrollee. “That means you will have the freedom to decide how you want to live your life,” says the WI DHS website. That freedom and independence is important to those who enroll in the program.

Preserving independence can be crucial for older individuals and people with disabilities. According to an article in the International Journal for Equity in Health, “Preservation of independence is among the most important health priorities cited by older adults” (Enogela, Buchanan, et al 2022). Additionally, less independence can lead to increased depressive symptoms in patients with spinal cord injuries and vice versa (Monin, Schulz, et al 2015). We all want to keep our independence and ability to care for ourselves as long as possible. The IRIS program provides more control for enrollees over their care and decisions affecting their bodies, homes, and lives.
Studies have also shown that aging-in-place, or allowing individuals to age at home, provides many benefits, including routine, comfort, and reduced physical and mental strain. The same holds true for those with disabilities. However, most healthcare insurance companies don’t cover the services and needs of older individuals or persons with a disability living in their home. The HCBS waiver allows IRIS enrollees to remain in their home and receive the necessary healthcare and other services, reducing hospitalizations and assisted living fees and preserving their independence.
The IRIS Difference
HCBS programs, such as Family Care (FC), Family Care Partnership (FCP) and the Program of All-Inclusive Care for the Elderly (PACE), use MCOs to coordinate care for enrollees. However, the IRIS program empowers enrollees by allowing them to manage their own care. They are given a budget based on their current needs and long-term goals, and they can spend that money however they see fit within the program’s rules and regulations. IRIS covers a variety of services and commodities, including in-home medical care, house cleaning, errands, assistive devices, and more.
WI DHS’s IRIS website points out, “Joining IRIS does not mean doing things all by yourself. Others will help you along your way.” Others include an IRIS consultant and a fiscal agent, who can advise the enrollee on how to use the budget for current needs and adjust it when future needs arise.
Wisconsin’s IRIS program has over 25,000 people enrolled as of January 1, 2024 (WI DHS). Each individual selects an IRIS consultant agency (ICA) to work with—an important decision essential to smooth and safe service. How can enrollees effectively compare these organizations to determine which one is right for them? Enter MetaStar. MetaStar is essential in upholding IRIS program standards and providing user-friendly scorecards for each ICA, helping enrollees easily determine which ICA to work with.
MetaStar’s ICA Review Process
ICAs have different responsibilities to their participants than MCOs, resulting in different review processes. The IRIS program review focuses on the interactions between the enrollee, consultant, and ICA.
The MetaStar IRIS Record Review team, part of the External Quality Review Department, evaluates the six IRIS consultant agencies in Wisconsin. As noted in the previous blog post, this team is populated by former care workers, including social workers, nurses, and therapists who “come with direct experience in the field and really understand how the system works,” said Alicia Stensberg, MetaStar Project Manager.
The MetaStar IRIS Record Review team reviews over 400 ICA participant files quarterly, looking for a comprehensive care plan, monthly contact by the IRIS consultant with the participant, incident documentation, and other quality indicators. Data collected is converted into scorecards by WI DHS. “It’s a lot of oversight at the participant level to make sure their needs are getting met.” explains Stensberg. The MetaStar IRIS Record Review team helps to make sure the ICAs understand the metrics and requirements. They also provide technical assistance and help solve problems during the review process.
MetaStar’s team helps organizations address “not met” requirements by clarifying requirements, monitoring follow-ups, and documenting improvements. “We have a lot of contact with these organizations,” Stensberg said. “We also work closely with the state to make sure the ICAs are improving, and they are.” She notes that while immediate improvements may not be evident each quarter, significant long-term enhancements in the performance of the ICAs have been seen, which she attributes, in part, to the ongoing reviews.
Hotline for IRIS Participants
MetaStar also operates a hotline for IRIS participants to report grievances or complaints regarding the IRIS program. MetaStar employees staff the hotline during business hours. The MetaStar employee works with the participants and the agencies to find acceptable resolutions. “From a statewide perspective, the [number of] grievances is relatively low, less than 1% of the membership,” Stensberg said. “It’s a healthy amount. No grievances mean people aren’t exercising their rights.” The grievances reported during these calls do not affect the scorecard results.
The IRIS program supports Medicaid enrollees’ dignity and independence. MetaStar provides clear evaluations of the ICAs and a grievance hotline, ensuring enrollees’ care is taken seriously. It’s crucial to consider future medical and personal care—for oneself and loved ones. “Anyone can end up needing Medicaid benefits at any time,” Stensberg explains. She also reminds us that “one of the most important things that we can do as a society is take care of the people who are marginalized. It is our duty, and frankly, it would cost us a heck of a lot more if we didn’t.” Scorecards created by WI DHS with data from MetaStar’s experienced review team enable clear decision-making during difficult times and offer a way for WI DHS and MetaStar to help Wisconsin’s marginalized populations.
“Do not regret growing older,” said Mark Twain. “It is a privilege denied to many.” While we’re not entirely sure Mark Twain is the author of this adage, the truth in the statement still rings clear: aging is not a disease to be fought, but a stage of life to appreciate and possibly even enjoy. However, aging can also bring health issues, loss of ability, financial struggles, and lack of a support system. By 2040, the number of Americans age 65 and older will reach 21.6%, according to the Administration for Community Living (ACL), up from 16% in 2000. Additionally, people who are disabled—who make up almost 27% of the population according to the United States Centers for Disease Control and Prevention—experience similar challenges.
These groups of people often face challenges caring for themselves. While some lucky people can self-fund care in aging years or disability, many others lack the financial resources for these situations. While Medicare and private insurance can alleviate medical costs and replace lost wages, medical care isn’t the only need to arise when a person becomes unable to care for themself.
Medicaid enrollees receive medical care, but they also require support in their homes and communities for various tasks, including at-home medical tasks, personal care, home care, pet care, errands, and much more. However, most health insurances won’t cover these services outside of a medical setting. Older adults or people with a disability are then caught in a web of problems: Can they self-pay for care? Is there a friend or relative who can help them? Should they move to a nursing home or assisted living facility? Depending on the extent of needs, some of these options aren’t possible. Fortunately, Wisconsin offers various ways to meet the long-term care needs of older adults and people with disabilities while allowing them to stay in their own homes.
The Wisconsin Way of Meeting Long-Term Care (LTC) Needs
Wisconsin provides LTC services through Medicaid Managed Care programs, including Home- and Community-Based Services (HCBS), through the following programs: Family Care (FC), Family Care Partnership (FCP), and the Program of All-Inclusive Care for the Elderly (PACE). FC is offered statewide while FCP and PACE are only offered in certain counties. These programs, operated by managed care organizations (MCOs), provide a variety of healthcare and other services that allow people to remain in their homes. When a person enrolls in one of the HCBS programs, they need to choose an MCO to work with as care is coordinated through the enrollee’s team at the MCO.
Wisconsin has four MCOs. When an MCO plays such an important part in a person’s life, choosing the right one becomes essential. How can anyone compare such large and varied organizations? MetaStar helps maintain program standards and contributes data to user-friendly scorecards for each MCO. Potential enrollees can easily compare options and select the most suitable one based on impartial data that has been collected and reviewed by MetaStar.
MCO Scorecards—MetaStar Makes the Difference with Data
MetaStar’s Quality Compliance Review team conducts reviews annually to gather data for the MCO scorecards. The team reviews each MCO in the state. “It’s a comprehensive system-level evaluation to determine that they are meeting requirements and hopefully exceeding them,” said Alicia Stensberg, project manager for the External Quality Review Department at MetaStar. Data for the scorecard comes from program enrollee surveys, an extensive document review, and employee interviews, with the latter two completed by MetaStar’s team.
The MetaStar team reviews documents such as policies and procedures, monitoring data, training information, contracts, correspondence, and much, much more to ensure these documents meet the metrics set by the state and federal governments. Employee interviews conducted over two or three days, involving various groups of staff members—everyone from information technology to care team members to leadership to support and supervision staff gets interviewed. The interviews are done to corroborate the findings from document review, but Stensberg finds them interesting for another reason: “It’s neat to hear [the staff] talk about their passions for supporting members and helping people live full and safe lives. I hear about the different initiatives that they have and the ways that they’re being collaborative with different organizations and different resources, all in the name of supporting members. It’s a cool experience.” She cites an example of another state’s Medicaid program addressing gun violence, highlighting the importance of caring for enrollees’ needs beyond direct medical care. Stensberg continues: “If you’re looking at caring for the whole patient, gun violence is very, very real for so many of the Medicaid recipients. The amount of impact Medicaid has amazes me.”
Data from the review process helps reviewers identify a requirement as “met” or “not met.” If something is found to be deficient, Stensberg explains, the Wisconsin Department of Health Services (WI DHS) can implement a corrective action plan for the organization to make improvements.
The hundreds of pages of MetaStar’s technical review are distilled into key areas for MCOs, such as such as satisfaction, responsiveness, communication, care delivery, quality standard, staff turnover and staff ratios. The WI DHS compiles this data into easy-to-compare scorecards.
Additionally, the review data is reported to the Centers for Medicare & Medicaid Services (CMS) as an Annual Technical Report, which is hundreds of pages long (and available online for anyone who is interested.)
The MetaStar Quality Review Team
The Quality Reviewers are part of the MetaStar External Quality Review Department. Stensberg calls them “some of the most amazing people I’ve ever worked with. All of them are such strong advocates for the individuals receiving services and really understand how the systems operate.” They all have 10 years or more of experience in LTC or a related field, such as nursing, counseling, social work; they’ve worked with children’s programs and family care organizations. Stensberg herself previously worked with adults with disabilities, and, like the rest of her team, she thinks it helps her in her current work. While she misses the job, “I’m glad to be here because I’m still part of the field. I think I’m having an impact on a broader scale.” This all-star team ensures regular assessment of the MCOs so participants can be assured that the scorecards are a carefully considered collaboration between WI DHS and caring, patient-focused MetaStar reviewers.
In addition to the MCO reviews and scorecards, the External Quality Review Department is involved with another HCBS-waiver program: Include, Respect, I Self-Direct (IRIS). This unique program allows enrollees to have more control over what care they receive, where they receive it, and when. Be sure to check in next month when we discuss the IRIS program and its formula for giving enrollees more influence in the direction of their healthcare as well as more choice and more independence.
May is the American Stroke Association’s (ASA) American Stroke Month. Often unrecognized and untreated, strokes can have devastating consequences:
- Each year, nearly 800,000 stroke patients join the 9.4 million adults (20 years old or older) in the United States who have had a stroke and are living with its effects. Of those 800,000 patients, over 160,000 will die.
- One American has a stroke every 40 seconds, and one American dies of a stroke every 3.25 minutes.
- 40% of strokes in the United States occur in males, and 60% occur in females.
- The risk of having a first stroke is nearly twice as high for non-Hispanic Black adults as for White adults. Non-Hispanic Black adults and Pacific Islander adults have the highest rates of death due to stroke.
- Strokes rank fifth among all causes of death in the United States.
- In 2020 (the latest year for which data is available), 2,091 people in Wisconsin died of strokes.
• Strokes are the leading cause of disability in Wisconsin.
• About 25% of people who recover from their first stroke will have another one within five years.
• Up to 80% of strokes are preventable.
(Sources: Wisconsin Environment Public Health Tracking Program, The Centers for Disease Control and Prevention, Wisconsin Department of Health Services Coverdell Program, Stroke Awareness Foundation)
The cost of strokes in human lives and resources continues to grow each year. There’s no better way to mark this important awareness month than to discover the ways the Wisconsin Department of Health Services (WI DHS) and MetaStar are enhancing the continuum of care for stroke patients across the state.
The Quest for Better Stroke Care
Paul Coverdell was a Georgia Senator who died from an intracerebral hemorrhage in July 2000 while serving in Congress. He served the people of Georgia for nearly 17 years before his death at age 61.
This tragedy led to the creation of a new stroke care program. In 2004, the Centers for Disease Control and Prevention (CDC) established the Paul Coverdell National Acute Stroke Program in response to Senator Coverdell’s death and a three-year study on stroke care in the United States. The program provides funding to state health departments that are committed to improving stroke care.
Wisconsin’s community-based organizations, emergency medical services (EMS), hospitals, professional organizations (like the ASA and the American Heart Association [AHA]), academic institutions, public health, and industry partners work together to “ensure that all patients in Wisconsin receive timely, high-quality acute stroke care” (WI DHS).
MetaStar Meets Coverdell
Dot Bluma, BSN, RN, CPHQ, is MetaStar’s stroke project specialist. She provides invaluable support to the program. Bluma currently works with hospitals to analyze data, finding areas where more focus or education is needed. “I’m our data geek on this program,” she said with a laugh. “I’m a nurse, but I’ve become a data nerd.” She has three colleagues on the Coverdell team, one who works with EMS, and two others who work with community partners, all with the same goal of improving stroke care in Wisconsin.
Wisconsin Coverdell in Action
Though the broad focus of a Coverdell program is decided by the CDC, the awardee states can choose to work on specific areas anywhere along the stroke-care continuum that fit within the broader focus. Wisconsin has chosen several areas to focus on for the current program’s focus on disparities.
 “We always start with educating the community,” said Bluma. “How can we prevent a stroke from happening?” Educational materials created by the Coverdell team addressed that question. “Risk Factor Rick,” created in 2023, explains stroke risks and how to combat them. “BE FAST Bella,” created in 2017, educates about the signs of a stroke, using an acronym adapted from the ASA’s FAST acronym. With the most recent Coverdell program, the materials were translated into Spanish, Hmong, Somali, and Russian, which, along with English, are the languages most frequently spoken by stroke patients in Wisconsin. “We want to meet people where they are and be cognizant of everybody’s diversity,” Bluma said.
“We always start with educating the community,” said Bluma. “How can we prevent a stroke from happening?” Educational materials created by the Coverdell team addressed that question. “Risk Factor Rick,” created in 2023, explains stroke risks and how to combat them. “BE FAST Bella,” created in 2017, educates about the signs of a stroke, using an acronym adapted from the ASA’s FAST acronym. With the most recent Coverdell program, the materials were translated into Spanish, Hmong, Somali, and Russian, which, along with English, are the languages most frequently spoken by stroke patients in Wisconsin. “We want to meet people where they are and be cognizant of everybody’s diversity,” Bluma said.
Equally important is ensuring that when the patient goes home, their individual needs are met. In addition to medication, regular blood tests, and follow-up appointments, the Coverdell program provided the opportunity to begin including community resources in stroke recovery. Bluma described an integrated health program between the Milwaukee Fire Department (MFD) and Froedtert Hospital that refers certain high-risk stroke patients to the MFD Mobile Integrated Health Program (MIH). MFD performs home visits, assesses and addresses safety concerns, provides education, and more. MIH then sends a report back to Froedtert who enters the information into the database so outcomes can be studied. “It’s been a phenomenal connection,” Bluma said. ” Clients say it’s been worth its weight in gold.”
Decoding Coverdell Data
With so many areas that could be the focus of this much-needed program, how does Coverdell identify which areas should and could be targeted for improvement? They use data from the AHA’s Get With The Guidelines®-Stroke database. According to the registry, over 9.5 million patient records from over 3,400 hospitals have been entered. The database provides a rich data set for analyzing stroke care at the hospital, Wisconsin, and national levels. Factors like bed size, hospital certification, sex, and more can be analyzed and interpreted to improve the quality of stroke care. Bluma spends part of her time working in the database and helping hospitals with their data. EMS data can also be integrated into the Get With The Guidelines®-Stroke database to provide a fuller picture of patient care and transitions.
Additionally, Coverdell creates hospital report cards based on the Get With The Guidelines®-Stroke database. Hospitals can now easily compare their data and benchmarks with all Coverdell hospitals in Wisconsin and hospitals nationally. Similar report cards have been created for EMS as well.
The Future of Stroke Care
Bluma isn’t one to rest on her laurels. She continues to sift through data to identify ways to improve stroke care in Wisconsin. “Addressing disparities in stroke care is an area we need to have a bigger focus on,” explained Bluma. Through continued work by implementing evidence-based stroke care education and protocols to reduce geographic, racial, and ethnic disparities, MetaStar aims to pave the way for targeted approaches that address individual patient needs. Continuing to leverage the relationships between community-based organizations, emergency medical services, hospitals, and patients and families are crucial in successful pre and post stroke care. The ongoing approach is to continue to build on prior work, provide equitable and inclusive care to diverse communities, and leverage data and technology, to ensure the future of stroke care will be more equitable and effective.
